Anatomy of a Shortage: A Lack of Contrast Media Supplies Compromised Care for Up to 10 Percent of Patients in Key Clinical Categories

Key Takeaways:
- PINC AI™ data shows that up to 10 percent of hospital inpatients who should have received an advanced image as part of their recommended care did not due to a nationwide shortage of contrast media.
- When fill rates plummeted to under 10 percent of what was ordered, providers were forced to conserve supplies, which often meant limiting imaging services to medical emergencies only.
- Rationing of imaging services affected patients across clinical conditions that rely heavily on advanced imaging for diagnosis and surgical care, including COVID patients, mothers and babies, and hip/knee and spinal surgeries.
PINC AI™ data shows that up to 10 percent of hospital inpatients who should have received an advanced image as part of their recommended care did not due to a nationwide shortage of contrast media.
Contrast media went into shortage[i] in mid-April after COVID-19 lock downs in China halted the Shanghai-based production center responsible for nearly 80 percent of product for one of the two primary suppliers serving U.S providers[ii]. Premier fill rate data shows that the shutdown triggered an almost immediate dip in contrast media fill rates that persists today.

Source: Premier, Inc fill rate data
Premier leverages manufacturer data, member reporting and fill rate trends as mechanisms to help determine the health of the supply chain. For drugs, Premier considers a healthy fill rate to be above 90%, and anything that falls below 80 percent is an early indication that demand is outpacing supply and that shortages may be imminent.
During the shortage, providers were forced to conserve supplies, which often meant limiting imaging services with contrast media to medical emergencies only.
However historically, less has been known about exactly how many procedures are deferred due to a particular shortage, or the effects on patient care.
To determine the impact, PINC AI™ data scientists examined five clinical conditions typically reliant on advanced imaging with contrast media (COVID patients, mothers and babies, hip/knee and spinal surgical patients). The data showed deep drop offs in imaging utilization starting in April and continuing through the summer, when the contrast media shortage was most acute.
Looking just at computerized tomography (CT) scans, for instance, data show that as many of 10 percent of patients across clinical focus areas who were expected to receive an advanced image did not. Nationwide, the average number of patients who did not receive imaging services that would be typically expected hovered around 5 percent during April and May, and around 6 percent in July before finally recovering at the end of this summer.
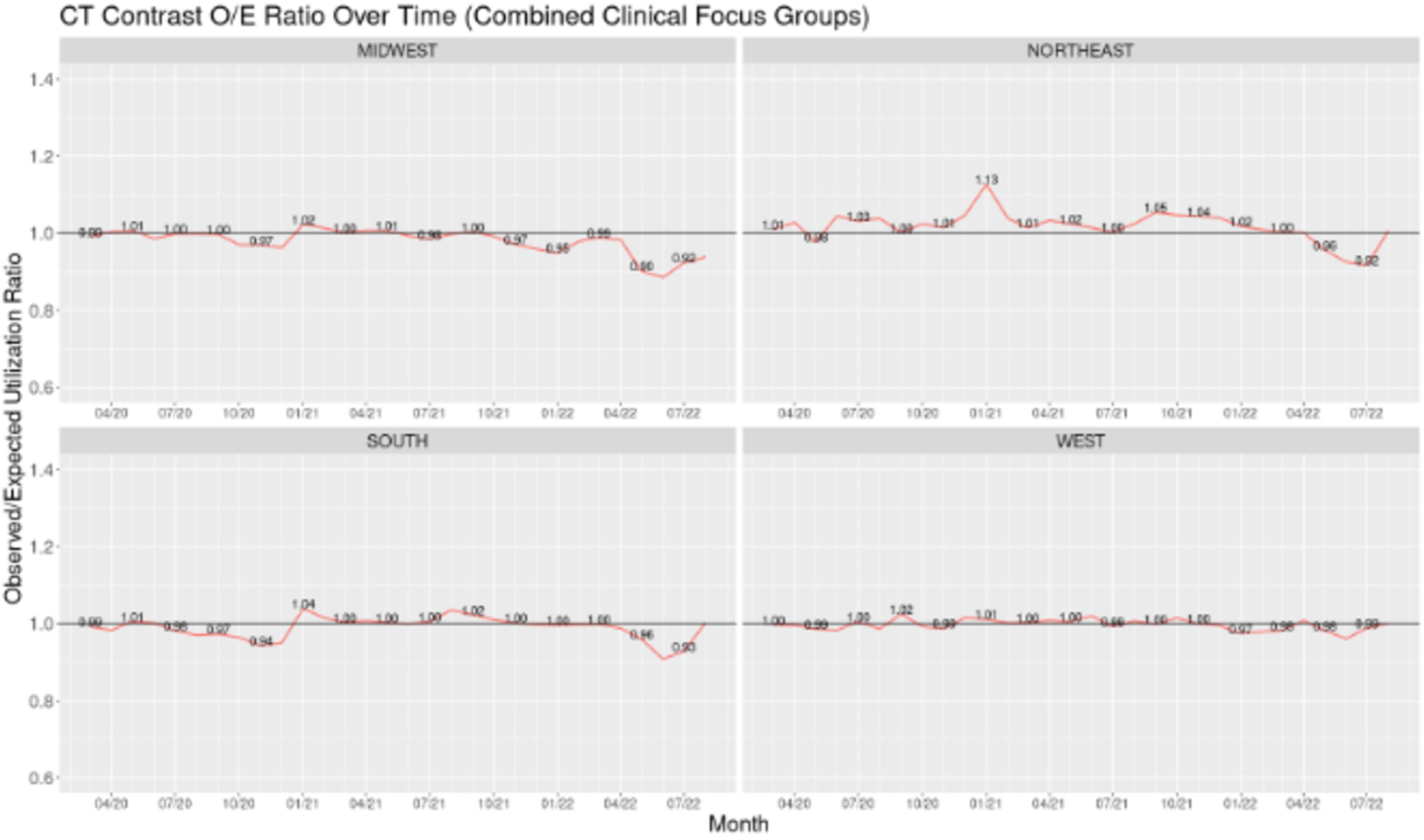
Source: PINC AI™ Healthcare Database (PHD)
Contrast media is commonly used to enhance the quality of advanced images such as CT scans and magnetic resonance imaging (MRI). More advanced than a typical X-ray, these images can depict bone as well as blood vessels, organs and muscle. Producing a highly detailed image, these technologies are often used to diagnose common conditions, detect tumors or other abnormalities and help physicians prepare for surgeries. An estimated 50 million imaging exams[iii] are conducted with contrast media each year.
Solutions for Managing Shortages and Preserving Quality Care
Premier is committed to helping protect members from shortages like contrast media, and providing access to the vital products they need to ensure continuity of care.
- Monitoring robust data, Premier provides early communication to both our members and the FDA on potential or impending shortages of any healthcare products, including contrast media. Following the Premier team’s engagement in early spring to share data and report the shortage, contrast media was added to the FDA’s shortage list – paving the way for waived prior authorizations and improved patient access. Premier and our members continue to advocate that the FDA make sourcing, quality, volume and capacity information publicly available for all medical products sold in the U.S. in order to improve transparency and support risk mitigation. A streamlined U.S. regulatory framework is needed that makes it easier to collect data, implement workarounds and guide conservation strategies for all products.
- With limited suppliers in the market, Premier engaged in complex negotiations with national suppliers to develop creative solutions to mitigate this ongoing problem. Knowing that a generic form of contrast media was on the verge of FDA approval, Premier worked with the manufacturer to understand the timeline for FDA approval, which was expedited due to Premier’s work to have contrast media added to the FDA drug shortage list as well as new statutory authority, advocated for by Premier in March 2020, that permits the FDA to expedite review of applications for shortage list drugs. This work culminated in July when Premier put this generic form of contrast media on contract, providing an alternative product choice to help spark healthy competition and provide a more stable, reliable supply for members. Working with the supplier, Premier gained early access to distribute contrast media to members through the Rapid Commit™ Program, thus giving members an alternative supply source so they could better weather the shortage while the overall market stabilized.
- During the contrast media shortage and overall, member health system and Premier Pharmacy and Med/Surg experts have continuously shared intelligence, mitigation efforts, clinical conservation strategies and best practices. Specifically, Premier produced guidance to help members extend their limited supply of contrast media through guidance on repackaging and expiration dating, as well as sharing guidelines for conservation prescribing. This cross-collaboration is vital to providing comprehensive guidance for providers to reduce shortage workarounds and support greater efficiency.
- Historically, health systems lacked the insights to pinpoint when a product might become short. Backed by artificial intelligence, machine learning and Premier’s clinical expertise, PINC AI™ technology delivers actionable intelligence that can help mitigate supply chain risk by alerting when the specific products a health system depends on are anticipated to become unavailable. The tool’s signaling capabilities can help providers increase preparedness and maintain operations to avoid quality issues or care delays.
- Premier’s Disruption and Disaster Preparedness team is orchestrating efforts required to prepare for and respond to disruptions that impact our nation’s healthcare system. Via a proactive approach and always-on relationships, the team is in continuous communication with global suppliers to ensure safety stock and monitor for risks, with specific focus on products critical to care and categories with unhealthy markets. This team also publishes a weekly product watch list – a ranked list of priority products to help members determine when/if they may need to begin preparing to shift purchasing to alternatives. Unique to Premier and compiled using our purchasing data and member input, the watch list is designed to help with contingency planning, providing advance warning of potential unhealthy markets and connecting members to resources that can help ensure continuity of care. This list is shared weekly with White House leadership to provide insights on backorders and potential shortages and advocate for priority transportation of critical products.
For more:
- See our new PINC AI™ analysis on how Europe’s energy crisis is exacerbating healthcare product shortage risks.
- Stay ahead of supply chain shortages. PINC AI™ Margin Improvement is ready to partner with you to help you increase preparedness and maintain operations to avoid quality issues or care delays.
- Learn more about Premier’s industry-leading Pharmacy solutions.
Methodology
Data
De-identified patient level data from the PINC AI™ Healthcare Database was utilized for this analysis. The dataset was limited to inpatient stays related to one of five clinical conditions, as defined by Centers for Medicare & Medicaid Services: COVID-19, mothers, babies, hip and knee arthroplasty and spinal surgery. Imaging modalities were the most prominent contrast-eligible imaging techniques across the evaluated clinical cohorts. The response variable was defined as the binary occurrence of contrast medium in the presence of a contrast-eligible image. Extracted data elements included a set of patient clinical and demographic characteristics comprised of length of stay, age, gender, race, point of origin, discharge status, MS-DRG, cost type and payor type. For evaluation purposes, CMS-defined geographic region was also extracted. The data was separated into baseline and evaluation datasets consisting of 190,854 and 523,044 inpatient stays respectively, across 801 distinct facilities. Baseline data was limited to discharges occurring in 2019, while the evaluation dataset was limited to discharges occurring between January 2020 through August 2022. Given the recency of the COVID-19 cohort, the baseline period was narrowed to discharges occurring between January through December 2020, while the evaluation period was narrowed to discharges from January 2021 to August 2022.
Methods
The baseline dataset was used to establish expected contrast utilization. Expected utilization, defined as the probability of a contrast-based imaging given the administration of a contrast-eligible image, is computed at the patient level using multiple logistic regression, thereby controlling for patient-level clinical and demographic characteristics. Models were stratified by clinical condition and geographic region for both imaging techniques. Observed and expected utilization was summed to the facility and month level and expressed as a ratio of total observed to expected utilization of contrast media. A Welch’s two-tailed t-test evaluated significant deviations between observed and expected utilization.
[i] https://www.aha.org/advisory/2022-05-12-shortage-contrast-media-ct-imaging-affecting-hospitals-and-health-systems.
[ii] https://www.reuters.com/business/healthcare-pharmaceuticals/ge-unit-boosts-medical-dye-output-china-covid-lockdown-cuts-supplies-2022-05-10.
[iii] https://www.nytimes.com/2022/05/26/health/dye-contrast-scan-shortage.html.

Jessica leads Premier’s pharmacy strategy and is focused on technologies, tools and other offerings that improve resiliency and affordability across the pharmaceutical supply chain.

Pam has more than 25 years of experience in supply chain and surgical services. She is responsible for the ongoing growth of all medical/surgical areas of Premier's GPO portfolio, including surgical services, nursing, pediatrics, continuum of care and cardiovascular services.

Drew is a Data Scientist on ITS team, working on a variety of projects with Premier teams across the organization. He leverages Premier’s robust technology suite and data, using ML/AI and other techniques, to develop new methods for products and ways to evaluate member performance.
Article Information

Jessica leads Premier’s pharmacy strategy and is focused on technologies, tools and other offerings that improve resiliency and affordability across the pharmaceutical supply chain.

Pam has more than 25 years of experience in supply chain and surgical services. She is responsible for the ongoing growth of all medical/surgical areas of Premier's GPO portfolio, including surgical services, nursing, pediatrics, continuum of care and cardiovascular services.

Drew is a Data Scientist on ITS team, working on a variety of projects with Premier teams across the organization. He leverages Premier’s robust technology suite and data, using ML/AI and other techniques, to develop new methods for products and ways to evaluate member performance.