Clinical Transformation: A Premier Framework for Engaging Physicians

Key takeaways:
- Healthcare organizations must actively work on their care delivery systems if they are to succeed in the evolving world of value-based care.
- For clinical transformation to work effectively and be sustained, physician engagement is a must.
- The Premier Physician Engagement Framework provides organizations with a proven, comprehensive roadmap to follow in their clinical transformation initiatives.
To thrive in a world increasingly moving toward value-based care and population health, health systems need swift, sustainable plans to improve the quality, safety and affordability of patient care.
Large-scale transformation of this magnitude requires a multi-disciplinary, team-based approach. However, healthcare organizations often undertake it without a clear understanding of how to engage one of their most important stakeholders: the physicians.
In some health systems, physicians may be viewed as independent third parties that can be difficult to work with, so the temptation is to “kick the can,” designing new operating models in a vacuum, engaging physicians at a later date. But the truth is that such procrastination is often a mistake, particularly since it is the physicians that have the critical relationships with patients, with the power to make or break any change effort. They also have the insights needed to create deep, meaningful change.
Premier’s experts have worked within and for numerous health systems over many years. In our experience, having a framework for engaging physicians can be very helpful to creating the proper alignment and ensuring the effectiveness and sustainability of transformation efforts.
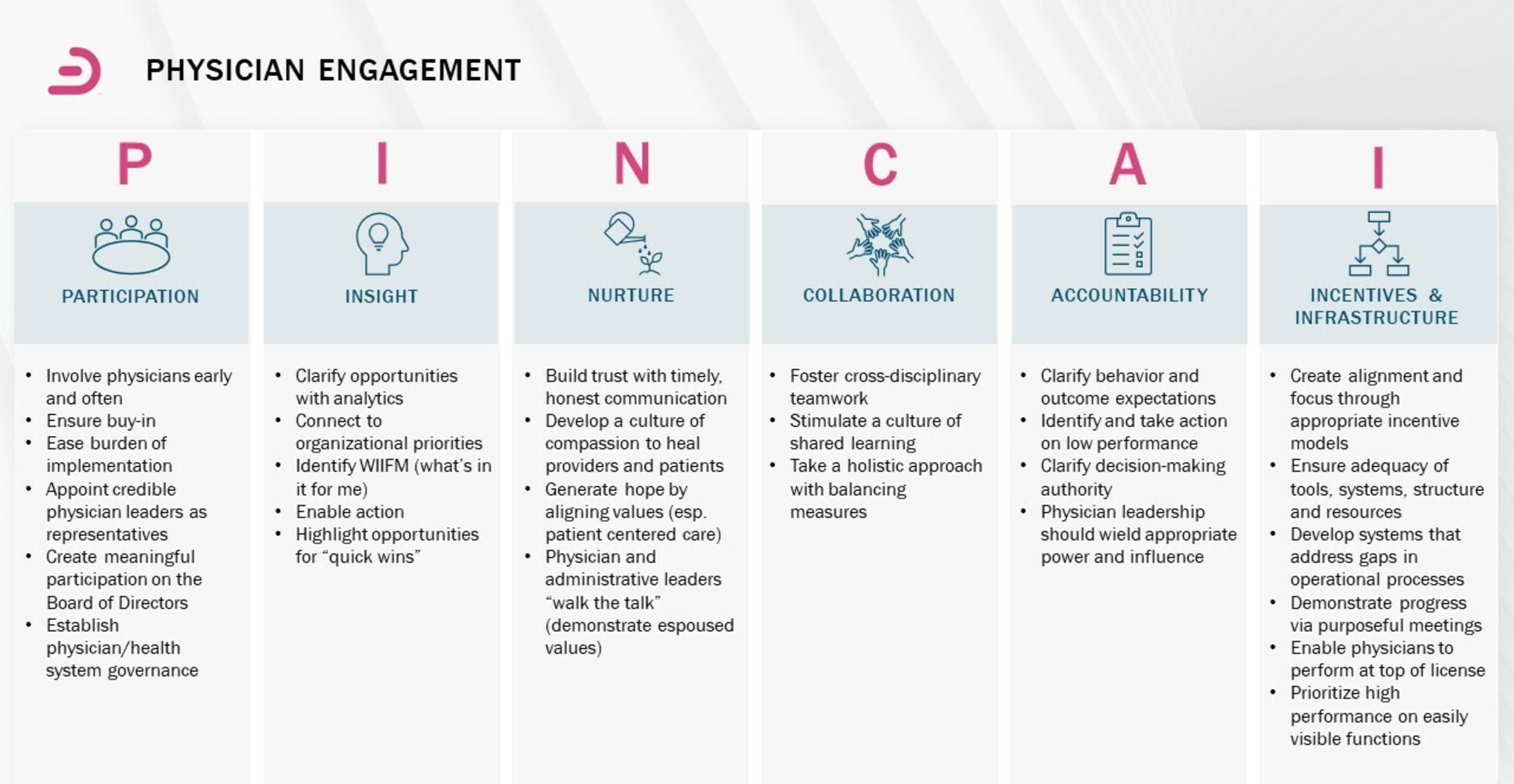
Engaging physicians can be thought of simplistically as developing a trusting relationship. But trust is not conveyed – it is earned. The Premier Physician Engagement Framework encompasses the essential activities that are needed to build a trusting relationship, including:
Participation
This requires making sure key physician stakeholders are invited, feel welcome and are actively involved. To start, we always advocate for transformation efforts to be co-led by both a system administrator and a physician, with inclusion of nurse practitioners and physician assistants as part of the overall team. Beyond the leadership structure, participation also involves creating feedback mechanisms to get the broadest possible insights into any change effort.
For instance, our experts often create a core cross-functional working group of 10 participants and ask that they send a survey to others on their teams based on the changes the core group has come up with for additional input, awareness and participation. This process can result in 90-100 individuals providing feedback, ensuring broad perspectives are taken into account and represented in the change process. Not only does it yield better results, it also helps clinical staff feel included in the changes to come.
Insight
Transformation works best when systems enable a “thinking environment” that caters to the physicians’ natural scientific bent. When they are encouraged to develop insights into what is and what is not working well, that will stimulate their thinking to help create and implement solutions as partners rather than as adversaries.
Our team of experts partners with physicians to undertake timely reviews of all relevant data that enables them to make informed decisions about changes to care practices, specifically linking outcome and efficiency metrics. For example, we don’t just tell physicians to use fewer vessel sealers in laparoscopic hysterectomy procedures. We instead show them the post-operative hemorrhage rates so they can drive their own insights and give them the outcomes information necessary to help physicians maintain or improve quality, while preventing waste or overuse.
Nurture
We recognize that many clinicians feel overworked, overwhelmed and overtaxed by the myriad requirements governing the practice of medicine. For transformation efforts to be successful, change initiatives can’t be viewed as just another thing to do, they must be meaningful and help address some of the core pain points that physicians experience every day.
Our teams typically take a two-pronged approach. First, we keep the patient at the center of transformation efforts, with all initiatives maintaining or improving patient outcomes and/or experience of care. When patient care is the north star, it can be used to maintain focus and help with conflict resolutions. Second, we work to make it easy for physicians to adopt changes by providing data and project management support, as well as hardwiring process changes into the electronic medical record (EMR).
Collaboration
Modern medicine is increasingly a team sport – and the same holds true with change initiatives. We find the most successful efforts are those that foster interesting new forms of collaboration for a stimulating, rewarding dynamic among all stakeholders.
For example, at one regional health system (23 hospitals), we helped physician leaders team up with their supply chain counterparts as part of the negotiation team working with suppliers to ensure more market-competitive deals. These deals addressed demand matching, utilization commitments and rebates. The program resulted in $2.2M in orthopedic implant savings and $400K in orthopedic trauma supply savings in the first year alone.
Accountability
Any successful system requires all participants to hold each other accountable for delivering results. This is not just about holding “them” accountable, but about creating systems in which we hold each other accountable. No one wants better results for patients than physicians, even though the ways in which this gets expressed may seem at odds with health system goals.
To encourage accountability, we develop comprehensive dashboards to track initiatives, which contain unblinded, physician-level performance against goals. This is often reviewed at service line or department meetings, which leads to physician-to-physician conversations that drive accountability for improved performance. In turn, we ensure that physicians are included in system-level governance, so they are able to hold executive leadership accountable for delivering on system-wide priorities.
Incentives and Infrastructure
For transformation to take root, it must be operationalized. This involves creating a set of tools, incentives, resources and structures that support engagement. Infrastructure is often overlooked, but in many cases, we have found that it is the environment and systems surrounding care delivery that are failing patients, not the individuals caring for them.
We have helped a number of clients implement co-management or gainsharing agreements with physicians to deliver significant improvement in targeted outcomes. Using these agreements, one regional health system (nine hospitals) demonstrated a $4M+ in projected revenue enhancement via improvement in emergency department (ED) throughput. Another urban medical center realized $600K in revenue enhancement through improved operating room (OR) block utilization. And a suburban medical center noted a two-year improvement in physician satisfaction from 27th percentile to 80th percentile.
Ready to jumpstart a clinical transformation in your organization? Learn more about how our experts experts can help.
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.
Dr. DeBehnke is a member of Premier's Advisory Services team where he leads consulting engagements in the areas of large-scale clinical transformation, clinical variation reduction and ambulatory operations improvement.
Dr. Gupta is an expert in care transformation, leading clinical variation, throughput and clinical redesign initiatives, as well as physician engagement and clinical governance functions to create a platform for sustainable change.
Article Information
Dr. DeBehnke is a member of Premier's Advisory Services team where he leads consulting engagements in the areas of large-scale clinical transformation, clinical variation reduction and ambulatory operations improvement.
Dr. Gupta is an expert in care transformation, leading clinical variation, throughput and clinical redesign initiatives, as well as physician engagement and clinical governance functions to create a platform for sustainable change.