Integrate Great: Best Practices for Aligning Owned, Leased and Managed Providers Within Your Health System

Key takeaways:
- Due to a variety of reasons including shrinking margins, staffing requirements, technology gaps, supply standardization and more, it can be challenging for health systems to integrate newly acquired providers in the care continuum.
- By focusing on five key areas, health systems can successfully align owned, leased and managed (OLM) providers within the care continuum and remain competitive in healthcare’s ever-changing landscape.
- With the combined expertise of our continuum of care (CoC) and performance services teams, Premier is creating new solutions to help health systems execute on the five key areas – optimizing the ambulatory enterprise for coordinated, quality patient care and cost effectiveness.
As the U.S. healthcare system continues on a consolidation trend, health systems face numerous challenges aligning and integrating newly acquired, leased or employed providers and practices into the care continuum. For example:
- Changes in reimbursement coupled with new technology are increasingly driving procedures into lower acuity settings of care.
- Downward margin pressures, staff shortages and increased patient access demands require new levels of standardization across practices and specialties to ensure the efficient use of resources and a reduction in both waste and variation in practice operations.
- Supply chain and clinical executives with continuum of care oversight must work together to achieve operational excellence in this environment.
The days of acquiring practices and leaving them alone is long gone. At Premier, we believe health systems must focus on five areas when aligning owned, leased and managed (OLM) providers across the ambulatory enterprise to improve overall performance and remain competitive in healthcare’s evolving environment.
Focal Area #1: Patient Access and Retention
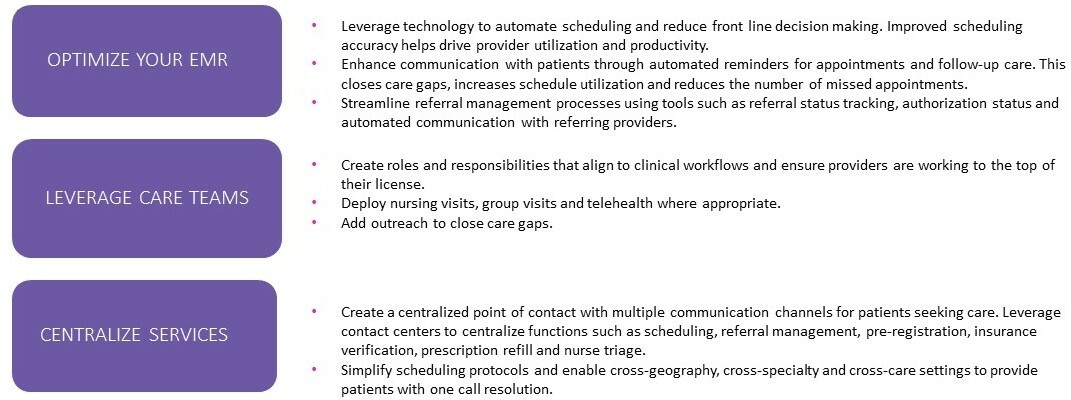
Patient access refers to the process of allowing patients to schedule appointments, access medical records and communicate with their healthcare providers. It’s a critical component of care delivery that can positively or negatively impact patient outcomes and the long-term success of providers. Three ways to boost patient access and retention efforts include optimizing the electronic medical record (EMR), leveraging care teams and centralizing services.
Focal Area #2: Provider Compensation Redesign
Transitioning provider compensation plans to the updated Centers for Medicare & Medicaid Services (CMS) work relative value unit (wRVU) table coupled with other compensation pressures are forcing medical groups to seek ways to redesign their compensation models without increasing total compensation spend, to ensure affordability. These efforts require updates to compensation plans between primary and specialty care, effective communication, shadow planning and a high level of provider education. Medical groups must assess the overall impact and weigh the right timing for their organization.
Creating a compensation model that aligns provider compensation with organizational goals can improve performance and financial outcomes by increasing physician engagement, motivation and productivity and promoting efficient resource utilization. Alignment can also enhance the quality of care by ensuring that quality and production incentives are equally valued and intertwined.
In our OLM provider integration work, we’ve seen organizations require providers to meet a minimum productivity threshold to qualify for any quality bonuses, and vice versa. Compensation models that support updating key performance indicators (KPIs) in the productivity and quality components allow organizations to continuously ensure alignment to organizational goals without a complete compensation redesign.
Focal Area #3: Clinician Standards
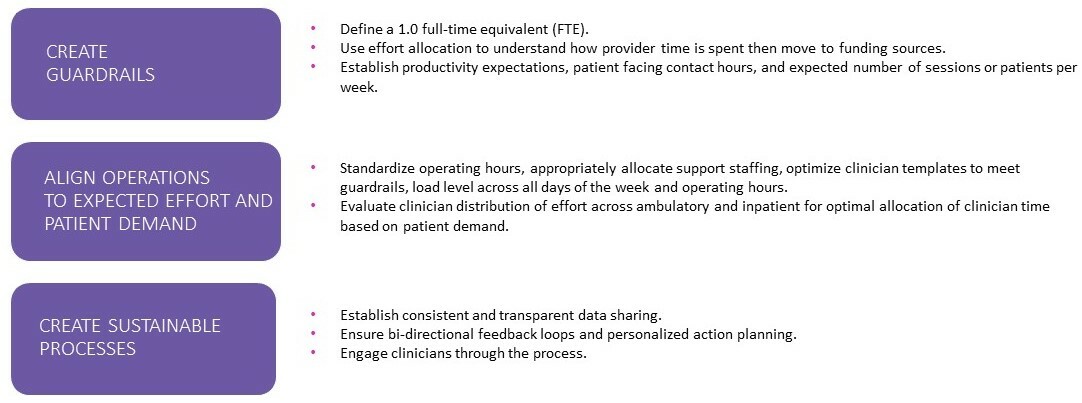
Establishing clinician standards and expectations across the ambulatory enterprise – underpinned by transparent data sharing – will help to increase efficiency, reduce provider variation of care and drive revenue enhancement to offset rising costs. We recommend a three-pronged approach that includes creating guardrails, aligning operations to expected effort and patient demand and creating sustainable processes.
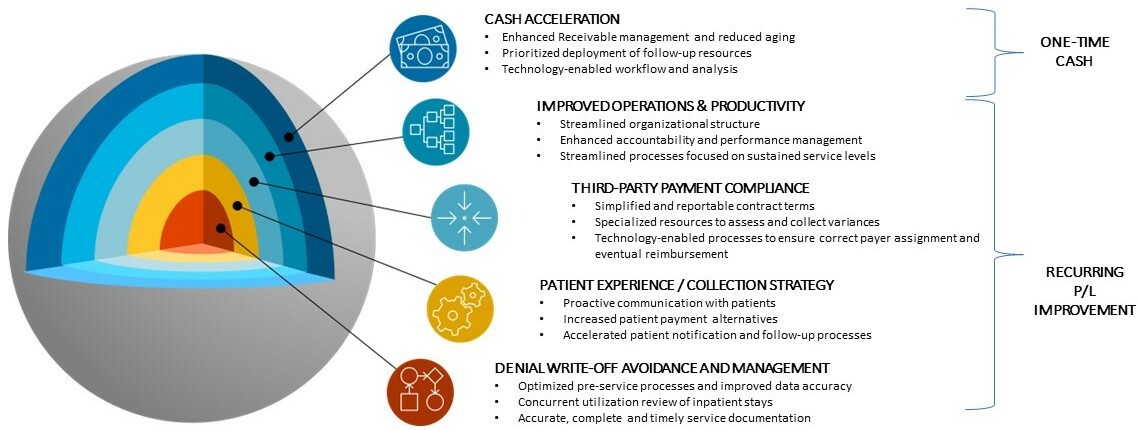
Focal Area #4: Revenue Cycle
Given the financial challenges health systems are currently facing, proper revenue cycle management is more important than ever. Below are five areas to consider for improving revenue cycle for both one-time cash acceleration and long-term sustainable change.
Focal Area #5: Supply Chain
Managing the supply chain across the non-acute CoC poses unique challenges for supply chain leaders. Unlike acute care, the non-acute supply chain is fragmented, with little to no centralized visibility, largely due to geographically dispersed locations that operate independently of one another and significantly more people placing orders for supplies. Supply chain operations must be carefully managed to drive down costs and improve financial performance while delivering high-quality patient care.
Here’s what’s needed to meet these goals and achieve benefits of scale:
- Leadership and knowledgeable staff to manage change.
- Technology to aggregate purchasing data and provide visibility and transparency into the supply chain across locations.
- Standardization of distributors, suppliers, products and services across the ambulatory enterprise.
Are you ready to put these five best practices to work in optimizing your health system’s OLM provider network?
Be sure to align with an experienced partner. Premier’s CoC and performance services teams are here to help:
- Maximize your purchasing power with our group purchasing organization (GPO) solutions, including 3,300+ negotiated contracts with industry-leading suppliers and more than $83B in combined annual purchasing volume for greater supply standardization and cost savings. Along with our GPO portfolio, Premier offers expertise in leveraging data, purchasing operations, and supplier and distributor relationships to help drive efficiencies across your enterprise.
- Technology-enable your supply chain with Premier SmartPO™, a digital procurement and inventory management platform that offers complete visibility into a provider’s purchasing process to help drive supply chain resiliency, savings opportunities and quality patient care across the care continuum.
- Manage the operational, financial and strategic performance of employed physician networks with our PINC AI™ InflowHealth solution, which provides data, analytics, dashboards and advisory services that engage and align efforts at all levels and roles of the medical group.
Through our solutions that help reduce purchasing costs, ensure providers have access to the right suppliers and products, provide full purchasing visibility, and tackle medical group operational and financial challenges, Premier is creating a more connected and efficient care continuum, which ultimately benefits health systems, providers and the patients they serve.
For more on this topic:
- Attending the IDN Summit? Register for our Lunch N Learn session on August 28 at 11 a.m. – Future-Proofing Your IDN: Adapting to the Continuum of Care Shift.
- Check out our blog to see four ways we’re breaking down silos to build a unified CoC.
- In another blog, deep dive into Premier SmartPO™ plus discover two additional ways Premier is tech-enabling the CoC to optimize the healthcare delivery system.
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.
During her consulting career, Kearin has delivered large integrated consulting engagements in community systems, academic health systems and standalone specialty hospitals across the U.S. Her areas of expertise include medical group operations and financial performance, strategic plan development, change management, leadership and organizational structure redesign, and physician governance creation/redesign.
Charlotte leads the strategy development of new initiatives for Premier’s Continuum of Care.
Article Information
During her consulting career, Kearin has delivered large integrated consulting engagements in community systems, academic health systems and standalone specialty hospitals across the U.S. Her areas of expertise include medical group operations and financial performance, strategic plan development, change management, leadership and organizational structure redesign, and physician governance creation/redesign.
Charlotte leads the strategy development of new initiatives for Premier’s Continuum of Care.