Joint at the Hip (and Knee): A Look Back and Ahead for CJR Hospitals
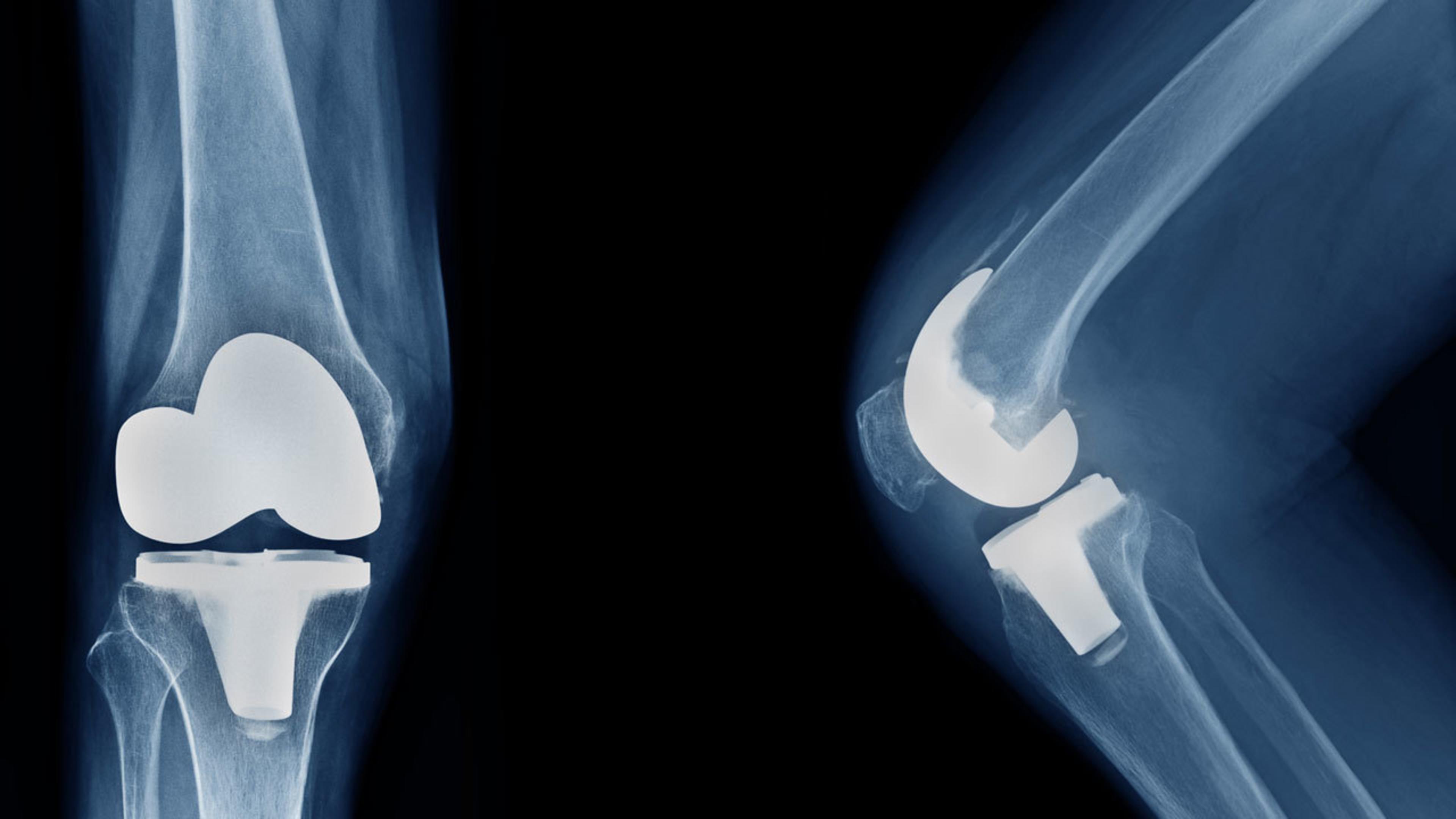
Optimizing pre- and post-acute management of beneficiaries is taking on increased importance throughout the Comprehensive Care for Joint Replacement (CJR) extension period. Providers are simultaneously navigating the effects of COVID-19, the migration of total knee arthroplasty (TKA) procedures to ambulatory surgery centers (ASCs) and the reintroduction of financial risk within the model.
To successfully navigate change in the final three years, it’s important to understand where CJR participants have been focused in the past.
Driving Success in the First Five Years
During the first five years of the model, CJR participants that joined Premier’s Bundled Payment Collaborative (BPC) have outperformed other providers in CJR in terms of quality and savings.
- More than 75 percent of Premier’s CJR participants earned excellent or good quality scores, resulting in a 1.5 percent or 2 percent discount rate, respectively, as compared to the standard 3 percent discount.
- In Performance Year 4, members of Premier’s BPC earned 70 percent more in net payment reconciliation amounts (NPRA) than other CJR participants.
How have these CJR participants achieved success? They have all adopted one or more of the following tactics:
- Pre-admission Optimization: Many CJR participants have discovered that the key to managing patients’ post-acute needs is to address them prior to surgery. To anticipate needs, Premier members have used concepts such as coordinating post-acute care (PAC) prior to admission, identifying potential social barriers for recovery and optimizing chronic conditions prior to surgery.
- Appropriate Post-acute Care Utilization: A major driver for decreased cost and improved quality in bundled payment models is the reduction in unnecessary PAC utilization. Premier members have been able to successfully identify circumstances in which beneficiaries could be appropriately placed in a lower cost setting while maintaining or increasing quality. This was accomplished by educating patients and surgeons about appropriate PAC settings and providing earlier physical therapy evaluation and intervention during the acute stay.
- Post-acute Follow-up: CJR participants have also assigned care coordination staff who follow up with patients throughout their 90-day PAC journey. This follow up covers everything from coordinating post-surgery office visits to identifying and addressing gaps in care.
Managing the CJR Model Extension
With the three-year extension of CJR in place, sustaining these strategies will be key. Furthermore, CJR participants will need to excel and expand their capabilities in other areas to be successful in the three-year extension period, including:
- Data Analytics: Both electronic health record-based and claims-based data are essential in driving success under bundled payment models. CJR participants will need to leverage this data to compare current outpatient TKA to inpatient rates in the region. As outpatient TKA can significantly impact target prices, keeping pace with the region will be important. Additionally, CJR participants will need to use this data to assess and address post-acute challenges with outpatient TKA, such as avoidable readmissions, emergency room (ER) visits and observation stays. Tools that assist CJR participants with evaluating not just their historical performance, but also how they compare to national and regional benchmarks, are critical.
- Care Optimization: The introduction of outpatient procedures and risk adjustment for individual beneficiaries will require CJR participants to focus less on overall care protocols and more on individual beneficiary needs. Prior to procedure, hospitals will be well served in identifying specific age and comorbidity barriers to achieve optimal outcomes for beneficiaries. Additionally, hospitals will need to focus more on post-procedure transitions such as ensuring patients are able to connect with specialists who are managing their comorbidities. Focusing on individualized care plans will both ensure patients are appropriately placed as inpatient or outpatient and will assist with readmission and ER utilization avoidance.
- Social and Health Equity Needs: Many CJR participants are nearing the point where traditional care redesign may have marginal impacts on improving quality and costs. Many organizations will find it beneficial to begin to incorporate beneficiary social and health equity needs into their broader CJR initiatives. This will require changing how post-acute patient care is evaluated. It is not enough to schedule post-acute follow-up; hospitals will need to identify barriers such as transportation, access and home support, which prevent beneficiaries from adhering to care.
The Centers for Medicare & Medicaid Services’ (CMS’) actions indicate that the agency is doubling down on a future that includes episode payment models.
Providers in the CJR model should take the time to carefully consider which aspects of their programs are working well and how they can continue to build upon their successes. CJR participants should build upon their historical strategies, such as post-acute network development, while using claims and electronic health record data to identify future opportunities in Year 6 of the model.
Our experts are helping healthcare providers successfully transition to value-based care models. Premier’s collaborative members have performed up to twice as well as providers in other bundled payment programs.
Learn more about how our Bundled Payment Collaborative is reducing costs, increasing savings and improving outcomes for our members.
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.
Kevin has more than a decade of experience in healthcare consulting. At Premier, he manages the analytic offerings for the Bundled Payment Collaborative and serves as a subject matter expert in episodic value-based care models.
Austin supports health systems participating in bundled payment programs by providing education, support on episode development and identification of cost reduction opportunities.
Article Information
Kevin has more than a decade of experience in healthcare consulting. At Premier, he manages the analytic offerings for the Bundled Payment Collaborative and serves as a subject matter expert in episodic value-based care models.
Austin supports health systems participating in bundled payment programs by providing education, support on episode development and identification of cost reduction opportunities.