Mechanical Ventilation Adds 5X the Cost to COVID-19 Care

According to a new Premier analysis, the cost for healthcare providers to treat a COVID-19 patient who is mechanically ventilated is more than five times higher than a COVID-19 patient who does not receive this treatment.

Additionally, the cost of mechanical ventilation for a COVID-19 patient is more than 1.6 times higher than the cost to mechanically ventilate a patient with other medical conditions. According to the analysis, mechanical ventilation for other conditions typically averaged $40,100 – almost 40 percent less than the cost to ventilate a COVID-19 case.
Drivers of Added Costs
Mechanically ventilated patients tend to be among the most ill, requiring a longer inpatient length of stay (LOS), which drives up resource utilization and costs.
According to Premier’s research, COVID-19 patients receiving mechanical ventilation have an average length of stay of 16.8 days, versus 6.8 days for COVID-19 patients who do not require ventilation, and 10.8 days for patients receiving mechanical ventilation for other conditions. By comparison, the Agency for Healthcare Quality and Research estimates the average length of stay for all hospital visits is 4.6 days.

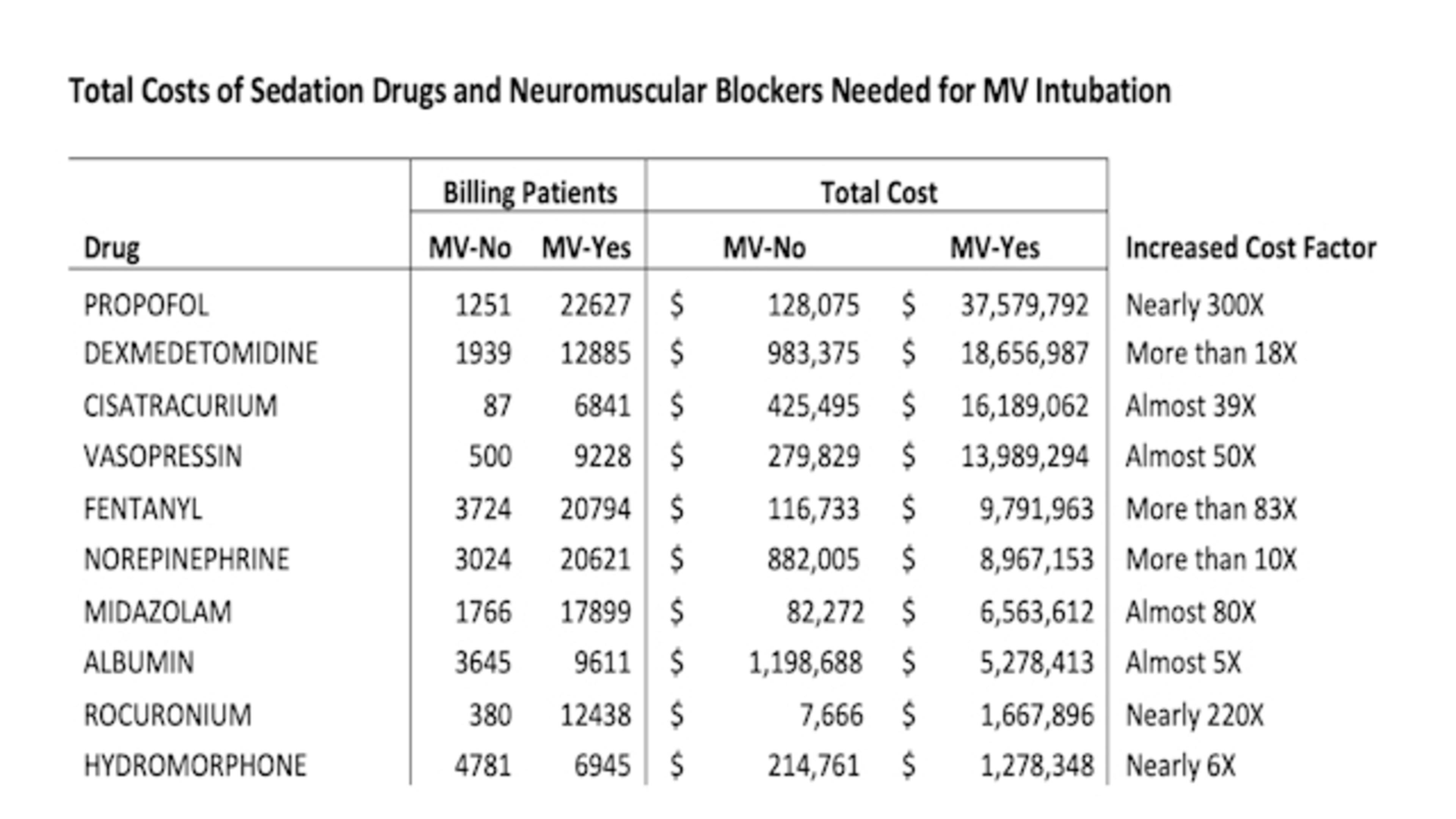
The bulk of the cost differential between mechanically ventilated COVID-19 patients and all others comes from the additional use of drugs, particularly sedatives and neuromuscular blockers that are necessary to alleviate the pain and anxiety associated with intubation. Total added costs for drugs range from 5X-300X for COVID-19 patents receiving mechanical ventilation versus COVID-19 patients who do not, driven by greater utilization costs on a per patient basis, as well as greater total volume.
Comparing the drug costs of mechanical ventilation for COVID-19 patients versus those with other conditions, costs were still an average of 42 percent higher, largely driven by increased drug utilization associated with a longer length of stay.
The Challenge with Stabilizing the Supply of Drugs in High Demand
Not only does mechanical ventilation increase total costs for the hospital to provide care, but it also represents a supply chain challenge. Many of the common, first-line sedation drugs needed for ventilation have experienced historic supply shortages or have gone into spot shortages across the country as COVID-19 cases increase.
Premier® data shows that demand for many of these drugs surged dramatically over historic volumes during the pandemic. Although the current supply for most of these drugs has stabilized and fill rates appear to be meeting need thus far, the drug supply chain remains fragile. If there is a dramatic uptick in demand due to an increase in COVID-19 cases requiring ventilation, the nation could once again experience shortages of these drugs.
Following the latest evidence for mechanical ventilation will be critical to improving patient outcomes as COVID-19 cases continue to climb across the United States. Health systems may also want to consider early conservation of drugs critical to support mechanical ventilation to ensure ample supply during a caseload surge. Many providers – 88 percent, according to a recent Premier survey on stockpiling pandemic medications – are increasing on-hand supply of these medications to ensure at least one month of surge demand, with some collecting up to 60- or 90-days of supply.
For its part, Premier has sourced a reliable supply of propofol, dexmedetomidine and hydromorphone through its ProvideGx® program – with plans to bring additional drugs necessary for COVID-19 care to market this year. ProvideGx works with manufacturer partners to increase production and secure three-to-six-month safety stocks of product in return for long-term, committed contracts with participants. During the pandemic, the model has been tested and proven highly effective. Since March, the ProvideGx program has weathered demand increases of 150 percent or more – with no interruptions in supply.
Learn More
- Download the full white paper: Margin of Excellence: Mechanical Ventilation Adds Significant Costs to COVID-19 Care
- Check out how ProvideGx is ensuring access to drugs at risk for shortage during the pandemic.
- Stay on top of the latest clinical guidelines for COVID-19 patients at the Premier Safety Institute®.
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.

Wayne is responsible for the contracting relationship with the pharmaceutical industry, including manufacturers, distributors and wholesalers, pharmacy technology and services, plasma derived products, vaccines and biosimilars.

Jessica leads Premier’s pharmacy strategy and is focused on technologies, tools and other offerings that improve resiliency and affordability across the pharmaceutical supply chain.
Article Information

Wayne is responsible for the contracting relationship with the pharmaceutical industry, including manufacturers, distributors and wholesalers, pharmacy technology and services, plasma derived products, vaccines and biosimilars.

Jessica leads Premier’s pharmacy strategy and is focused on technologies, tools and other offerings that improve resiliency and affordability across the pharmaceutical supply chain.