PINC AI™ Data: CMS Data Underestimates Hospital Labor Spending

Key takeaways:
- CMS updates hospital rates based on a wage inflation index that represents historical data. For FY 2022, this resulted in hospitals receiving only a 2.7 percent rate increase, compared to a 6.5 percent increase in hospital labor rates, according to PINC AI™ data. Labor costs account for nearly 68 percent of hospital costs in calculating the IPPS payment update.
- For FY 2022, CMS’s estimates of hospital spending growth using historic data represented less than the actual growth in the prices paid by hospitals for labor, supplies and services.
- The data CMS uses to account for real inflation in the cost of labor and other expenses is unlikely to reflect reality and produce an accurate payment update for the FY 2023 IPPS rule, due this spring.
For more on this topic:
- Read the hospital group letter signed by Premier, recommending sequestration relief for providers.
- Read a second hospital group letter signed by Premier, recommending additional provider relief funds be allocated to hospitals and health systems.
Later this spring, the Centers for Medicare & Medicaid Services (CMS) is expected to release proposed rules for the Inpatient Prospective Payment System (IPPS). For the FY 2021 and FY 2022 rules, CMS applied upward payment adjustments of 2.4 and 2.7 percent, respectively.
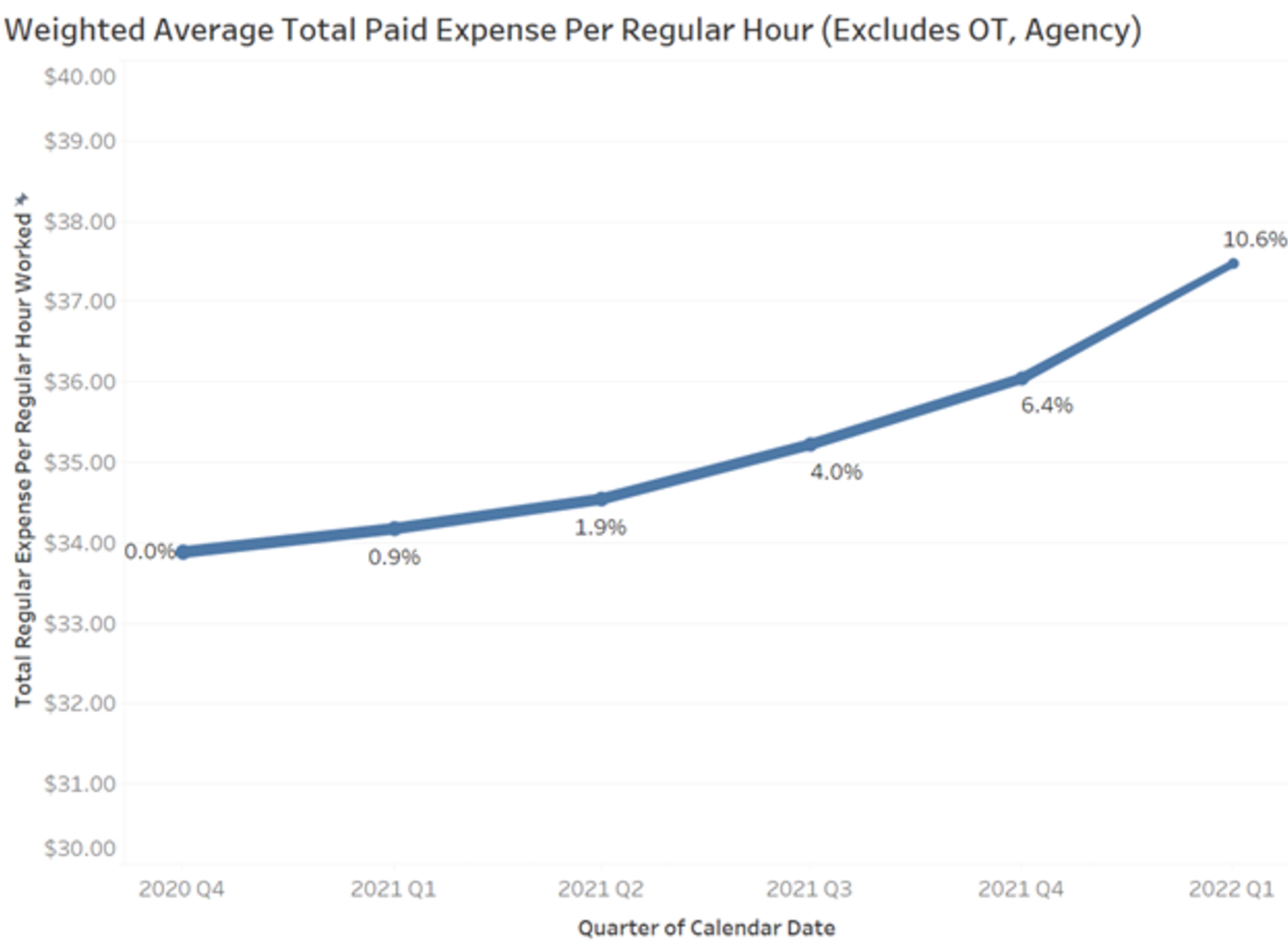
However, a recent PINC AI™ analysis finds that CMS’s payment adjustments did not adequately address hospitals’ increased costs. According to new data, hospitals’ labor rates alone jumped 16.6 percent on a per-paid-hour basis since Q4 2020 (start of government FY 2021) and do not show signs of slowing. Labor makes up about 67.6 percent of the CMS market basket calculation used to adjust hospital payments. A very high payment update in FY 2023 will be needed to match the rates most acute care providers are now paying their staff.

Importantly, these costs do not appear to be exclusively COVID-19 pandemic-related or transitory. Long before the pandemic, many clinical staff were in short supply and growing closer to retirement age. According to pre-pandemic research published in 2018, healthcare was projected to be short more than 1 million nurses by 2020 as a result of nurse retirements, an aging U.S. population and a stagnant talent pipeline. Since that time, the pandemic has only exacerbated matters, with more than 500,0000 nurse retirements expected in 2022. In fact, latest research from JOLTS/BLS indicates that there are 2.7 open positions for every one position filled. As talent shortages become more severe, providers are paying more to attract and retain scarce staff, a reality that is not expected to slow down as the pandemic subsides.
In fact, even removing use of temporary agency labor and overtime expenses that may have been more readily used to manage pandemic surge, inflation for labor expenses is still up 10.6 percent since Q4 2020.
Moving into the third year of the pandemic, our nation’s hospital and health system workers have cared for more than 4 million COVID-19 patients. At the same time, patient acuity and length of stay have increased when compared to earlier in the pandemic. These challenges are compounded by ongoing delays in non-emergent procedures and increased costs for supplies, medicine, testing and protective equipment.
Exacerbating the problem is the fact that relief from the 2 percent sequestration cuts has also expired, replaced by 1 percent cuts from April to the end of June, followed by a full resumption of the cuts by July 1. The net effect would be to add insult to injury – holding payment to below the actual increases in costs when many acute care providers are struggling to stay afloat after years of COVID-related financial losses.
As a result, it is imperative that CMS and Congress take action to ensure hospitals are adequately compensated. CMS should account for these expenses appropriately as part of its proposed IPPS rule update, due sometime this spring. Congress should also place a moratorium on the sequester, make additional provider relief funds available and provide additional time to spend provider relief funds previously distributed.
Methodology: To determine changes in hospital labor expense rates, PINC AI™ analyzed the data within its workforce optimization solutions, one of the nation’s largest and most robust sources for geographically diverse productivity data and benchmarks – all collected and validated by health system users daily. Paid Expense (Excluding Bonus) and Paid Hours figures are provided to PINC AI™ by its client health systems. The database of more than 1,400 hospitals was filtered to include only hospitals that provided both of these figures accurately for the same quarter, resulting in a representative sample of 580 hospitals across 110 health systems. For each quarter, the sum of Paid Expense (Excluding Bonus) was divided by the sum of Paid Hours, resulting in the Weighted Average Paid Expense Per Paid Hour figure shown in the chart. The value of this figure for each quarter was compared to the value for the initial quarter (Q4 2020) to calculate a percentage increase.
Paid Expense (Excluding Bonus) includes the wages for all salaried and hourly employees, including overtime but excluding bonus and other incentive payments. Expenses paid for contracted employees are included if provided by the health system. Paid Hours includes all worked, vacation, sick and other PTO hours for which the worker was paid. These two figures, and the resulting Weighted Average Paid Expense Per Paid Hour figure, provide the most direct comparison to the Employment Cost Index (ECI) used by CMS when determining the percentage change in hospital per-unit labor costs for the annual IPPS payment update. For FY 2023 IPPS proposed rule, the ECI data will include historical data through Q4 2021 and forecasted data for Q1 2022. The final rule will use updated data that includes historical data through Q1 2022 and forecasted data for Q2 2022.
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.

In her role, Aisha Pittman leads NAACOS’ work to promote legislative and regulatory policies that will advance ACOs.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.
Article Information

In her role, Aisha Pittman leads NAACOS’ work to promote legislative and regulatory policies that will advance ACOs.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.