Premier Data Shows Hospitals Paying $24B More for Labor Amid COVID-19 Pandemic

As the delta variant pushes COVID-19 caseloads to all-time highs, hospitals and health systems across the country are paying $24B more per year for qualified clinical labor than they did pre-pandemic, according to a new Premier analysis. The analysis found that clinical labor costs are up by an average of 8 percent per patient day when compared to a pre-pandemic baseline period in 2019. For the average 500 bed facility, this translates to $17M in additional annual labor expenses since the pandemic began.
Overtime and Agency Staff Are Driving Up Labor Costs
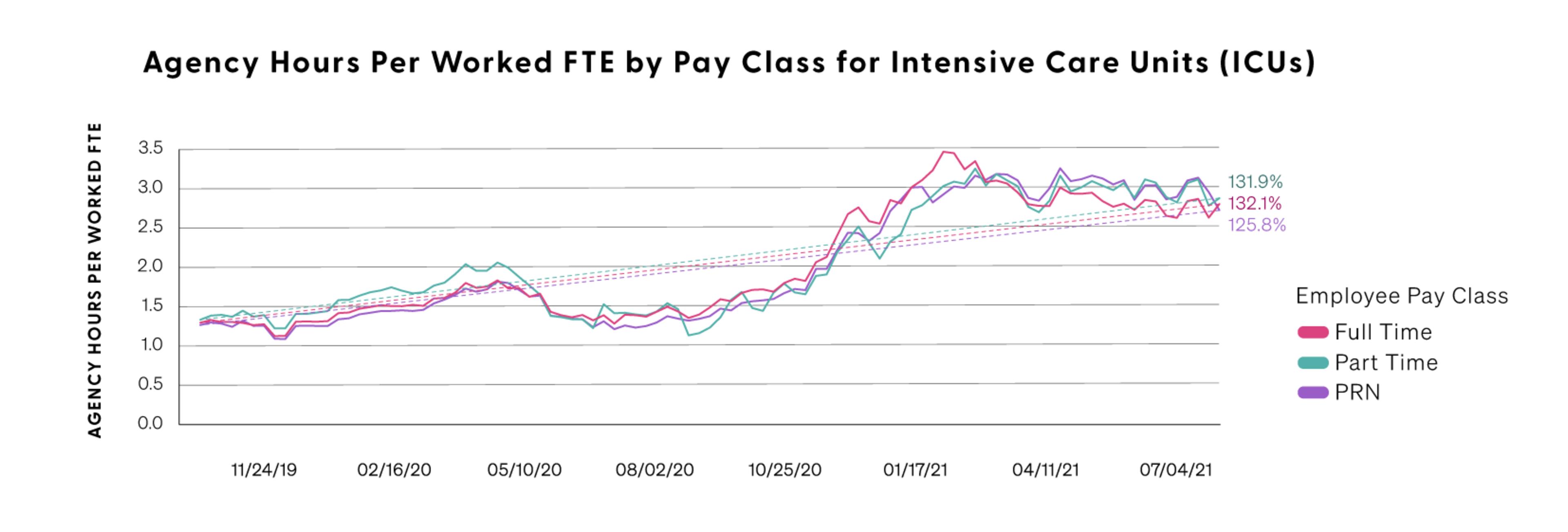
According to Premier data, overtime hours are up 52 percent as of September of 2021 when compared to a pre-pandemic baseline. At the same time, use of agency and temporary labor is up 132 percent for full-time and 131 percent for part-time workers. Use of contingency labor (or positions created to complete a temporary project or work function) is up nearly 126 percent.
Overtime and use of agency staff are the most expensive labor choices for hospitals - typically adding 50 percent or more to a typical employee’s hourly rate.
Hospital workers aren’t just putting in more hours, they are also working harder than ever before. The Premier analysis shows that productivity, measured in worked hours per unit of departmental volume, increased by an average of 7 percent to 14 percent year-over-year across the intensive care, nursing and emergency department units. Observing increased overall staffing cost during a period of improved staff productivity highlights just how significant the increases in cost-per-hour have become.
Sick Time and Turnover Provide Additional Stressors
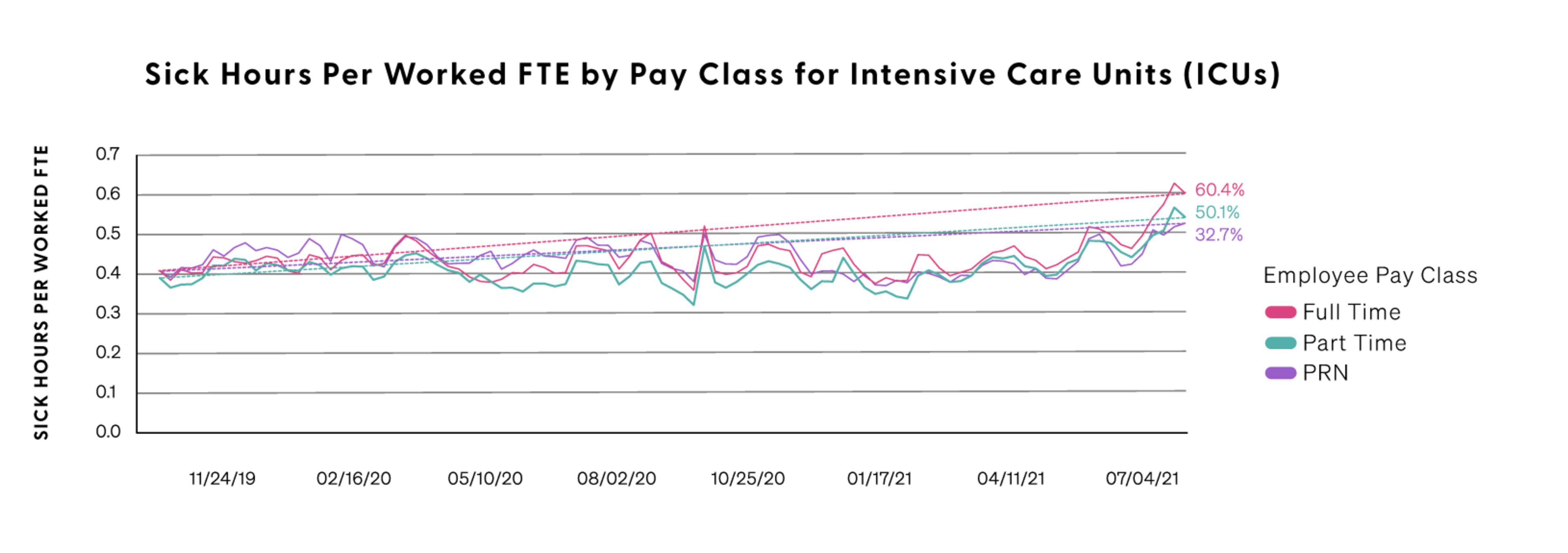
Hospital employees are more exposed to COVID than many other workers, with quarantines and recoveries requiring use of sick time. Premier data shows that use of sick time, particularly among FTEs in the intensive care unit, is up 50 percent for full-time clinical staff and more than 60 percent for part-time employees when compared to the pre-pandemic baseline. The combined stressors of working more hours while under the constant threat of COVID exposure are pushing many hospital workers to the breaking point. In fact, Premier data shows that clinical staff turnover is reaching record highs in key departments like Emergency, ICU, and Nursing. Since the start of the pandemic, the annual rate of turnover across these departments has increased from 18 percent to 30 percent. This means nearly one-third of all employees in these departments are now turning over each year, which is almost double the rate from two years ago.
This is a number that could increase as new vaccination mandates take effect. Already, one midwestern system reported a loss of 125 employees who chose not to be vaccinated. A New York facility reported another 90 resignations, and overall, staffing agencies are predicting up to a 5 percent resignation rate once vaccine mandates kick in. While a minority of the overall workforce, losses of even a few employees during times of extreme stress can have a ripple effect on hospital operations and costs.

Why We Should Be Concerned
According to the American Hospital Association, hospitals nationwide will lose an estimated $54 billion in net income over the course of the year, even taking into account the $176B in federal Coronavirus Aid, Relief, and Economic Security (CARES) Act funding from last year. Added staffing costs were not addressed as part of CARES and are further eating into hospital finances. As a result, some are now predicting that more than half of all hospitals will have negative margins by the end of 2021 – a trend that could be dire for some community hospitals.
How to Manage Costs While Taking Care of Employees – The Premier Difference
There are myriad reasons for the high cost and short supply of qualified clinical labor – meaning that solutions need to be holistic and multivariate as well.
Predictive Models
Using data from over 650 acute care facilities nationwide, Premier leverages machine learning to predict whether a specific department will face a critical shortage of clinical staff within the next eight weeks. Considering that it often takes 30-45 days to fully onboard new clinical staff members, this predictive model could provide an early warning system, enabling health system leaders to take staffing action before a shortage occurs. The model may also be used to identify departments where current staffing is likely sufficient over the near term, enabling excess resources to be aligned with the areas of greatest need. The model has thus far achieved an 83 percent accuracy score with an AUC of 86 percent when tested on a random 10 percent data sample withheld from model training. This is strong performance according to two standard model evaluation techniques; however, it should be noted that true performance in the future for any predictive model can only be estimated.

Benchmarks for optimal staff performance
Premier can provide health systems with productivity benchmarks against specific peer groups to identify areas of sub-optimal performance. These data markers pinpoint areas or departments where leaders may need to adjust staffing levels based on skill mix, staff configuration, shift configuration, etc. to manage patient care demands.
Work Redesign
The pandemic exacerbated many common, pre-existing challenges that hospital leaders face, including ensuring optimal patient flow and operational efficiencies across departments. These combined with labor challenges require sophisticated and innovative solutions. Premier advisors are available to work with health systems leaders experiencing current and future challenges to assess opportunities and implement smart solutions that work.
Manage agency costs
Premier has national and local group purchasing contracts to help control the costs of FTE and/or contingent staff for both clinical and non-clinical assignments. With vast healthcare staffing industry insights and end-to-end talent solutions, our strategic suppliers guarantee ROI - evidenced by the fact that Premier has been able to achieve discounts of 10 percent or more on talent solutions throughout the pandemic.
Consider international labor
To help manage through the delta surge, the Biden Administration announced they will fast track visa and other approvals needed for foreign nurses to enter the country to help healthcare facilities that are on the front-lines of the pandemic response. Approvals are only sped up for those nurses that have a viable employment offer. Backlogs for approval are extensive, so providers that are concerned with shortages need to be thinking ahead and planning accordingly.
Methodology
To conduct the analysis, Premier compared workforce trends from October 2019 through August of 2021 using workforce data. This database contains daily data for approximately 250 hospitals, bi-weekly data for 650 hospitals and quarterly data for 500 hospitals, collectively representing most geographic and demographic segments. Workers included in the analysis were limited to clinical employees working in the emergency department, ICU or nursing areas. Titles included in the analysis included nurses (RNs, LPNs, etc.), paramedics/EMTs, infection control practitioners, patient educators and clinical coordinators. Non-clinical staff such as administrators or those in finance, food service, communications, marketing, etc., were not included.

Mike is focused on driving innovation in healthcare and leading the industry through transformation by co-developing solutions with key stakeholders to help healthcare providers deliver higher quality care at a better cost.

Doug has extensive experience in workforce management and has presented at numerous national and regional events on topics ranging from healthcare workforce management, waste and inefficiency, performance improvement and lean healthcare.

Beth is a Principal Consultant at Premier who specializes in helping hospitals and health systems create effective workforce management strategies.
Article Information

Mike is focused on driving innovation in healthcare and leading the industry through transformation by co-developing solutions with key stakeholders to help healthcare providers deliver higher quality care at a better cost.

Doug has extensive experience in workforce management and has presented at numerous national and regional events on topics ranging from healthcare workforce management, waste and inefficiency, performance improvement and lean healthcare.

Beth is a Principal Consultant at Premier who specializes in helping hospitals and health systems create effective workforce management strategies.