Premier Data: Healthcare Workforce Insights Heading into 2025

Key Takeaways:
- A new data analysis prepared by Premier’s advisory services team reveals that while annual growth in hospital labor expense slowed in 2024, it remains higher than pre-pandemic levels.
- Hospital average hourly wage rates have increased 34 percent since 2019; agency rates have increased 63 percent.
- While 2024 shows some favorable trends, much work remains. Read below and watch the full webinar to see how Premier members and customers are addressing workforce challenges head-on.
Labor costs and availability remain top challenges for healthcare providers as we head into 2025. A new Premier data analysis reveals that while annual growth in hospital labor expense has slowed, it remains higher than pre-pandemic levels.
“Our data is showing that labor costs have slowed significantly over the last year and a half … growing about 2.5 percent in Q2 of 2024,” said Michael Voss, Director, Advisory Services. The remarks and analysis were shared during Premier’s recent thought leadership webinar, “Transforming the Healthcare Workforce: Insights for C-Suite Leaders.”
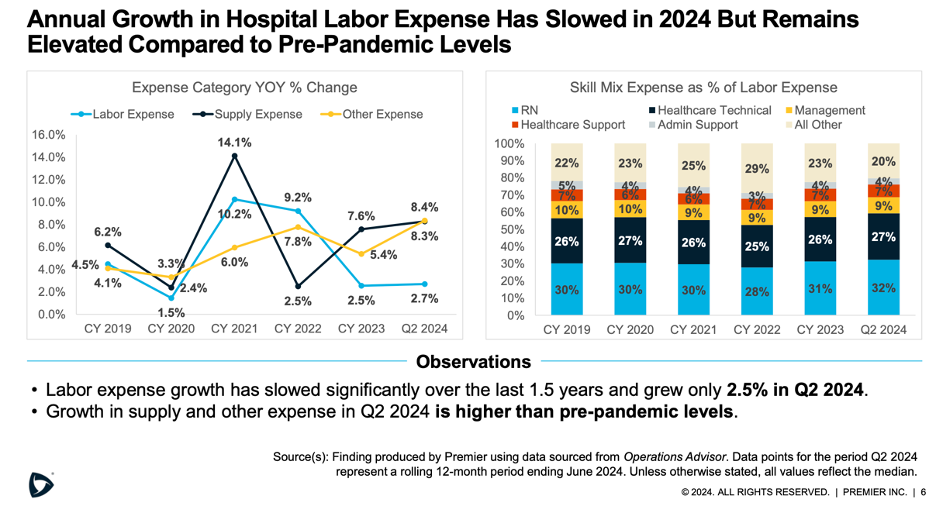
This trend in healthcare labor costs appears to align with broader U.S. labor costs, which, in the third quarter of 2024, recorded the smallest increase in over three years.
“While we’re seeing an increase in wage rates for all employees … they have also leveled off. We know that wage rates tend to be a lot ‘stickier,’ and once they go up, it’s a lot harder for them to come back down. As we look at opportunities to reduce workforce costs, reducing agency use and premium pay continue to play a key role,” said Voss.
Premier’s analysis found that while hospital average hourly wage rates have increased by 34 percent since 2019, agency rates increased by a whopping 63 percent in that same timeframe.

“Labor expense tends to be the largest expense for hospitals… when we look at the median year-over-year operating margin trend, margins have rebounded and are higher than pre-pandemic and historical norms. Of course, there are different factors contributing to that … among them include a hospital’s ability to manage labor costs,” Voss added.
Many Premier customer hospitals and health systems have begun to crack the code on reining in increased labor costs. Premier data shows that agency rates continue to decline since peaking in 2022. And when compared to 2022, agency rates have decreased 25.1 percent through Q2 2024. A few strategies have emerged as proven practices, including workforce benchmarking and streamlined governance; innovative recruitment and retention efforts; and establishment of structured workforce management offices (WMOs) to support workforce pipelines and resource allocations.
The Role of Benchmarking in Labor Cost Containment
Benchmarking for hospital-based care and services allows organizations to compare staffing levels and overall workforce strategies against industry peers. This enables them to identify areas for improvement, optimize resource allocation, reduce costs and deliver better patient care by leveraging proven, industry-wide practices and addressing potential staffing gaps.
“By developing a strategy for benchmark performance improvement, it allows you to focus on the 20 percent of the departments that represent 80 percent of the opportunity. Using this approach in concert with our process improvement efforts has led to significant, six-figure labor cost savings.” – Lance Bombard, Decision Support Analyst, Samaritan Medical Center (Watertown, NY)
Recognizing the organization’s unique capabilities is also a critical part of the benchmarking process, as is the use of quality-driven peer group comparisons. The latter includes the Centers for Medicare & Medicaid Services (CMS) Star program, Hospital Value-Based Purchasing (VBP) Program and nurse-sensitive outcomes.
Evolving Approaches to Recruitment and Retention
Effective recruitment and retention practices impact workforce stability, operational efficiency and patient care quality by ensuring healthcare facilities have access to enough skilled professionals.
While leveraging supplemental staffing through external agencies may provide short-term solutions, the long-term cost may include impacts on care quality. A recent study suggests that use of agency staff was significantly and negatively associated with six of eight quality measures, including hospitals’ HCAHPS star rating, the Hospital Compare rating and others.
Recruitment strategies vary by market and can sometimes be driven by competition across industries.
“… it can be challenging in our market, particularly with IT roles … we have a lot of competitiveness with attractive organizations like Amazon. We are creative about how to entice individuals to join the healthcare industry and get them to commit to joining an organization where we can match their skills with competitive rates of pay to meet the needs of our community and hospitals.” – Bethany Leland, Program Manager, Workforce Optimization & Operational Excellence and Lean Project Manager, EvergreenHealth (Kirkland, WA)
Programs and tactics such as nurse residencies, flexible and self-scheduling, tech-enabled talent sourcing, and streamlined interview and selection processes all seem to be having an impact. According to a recent report, hospital vacancy rates have improved dramatically. In 2024, 40 percent of hospitals had an RN vacancy rate under 7.5 percent, compared to just 12 percent of hospitals in 2023.
The Emergence of Workforce Management Offices to Execute Long-Term Operational Strategies
Establishing a WMO can be an effective means to address talent pipelines, recruitment and retention, short-term staffing solutions, and strategic workforce planning, among other areas. The WMO model has already had significant impact on both recruitment and reduced agency spending for University Hospitals Health System (UHHS).
“In terms of clinical agency spend … there is a saying in medicine that we cannot focus on the symptoms; we must focus on the cause. And clinical agency spend is a symptom of the situation that we’ve been in. Our focus has to be on recruiting and retention.” – Tom Conner, RN, MBA, System Director for Nursing Operations, University Hospitals Health System (Cleveland, OH)
Supporting ongoing recruitment for nursing assistant 2 (NA2) positions, designed for students enrolled in RN programs, is one function of the health system’s WMO. The UHHS WMO team found that between 50 and 60 percent of NA2 employees converted to RNs.
Over the years, the WMO worked with UHHS recruiting services to prioritize hiring RN students earlier in their studies. “Starting them in the hospital environment early in their schooling may help them determine whether they really want to be a nurse,” said Conner.
Hospital Leaders Share Their Top Concerns and Outlook for 2025
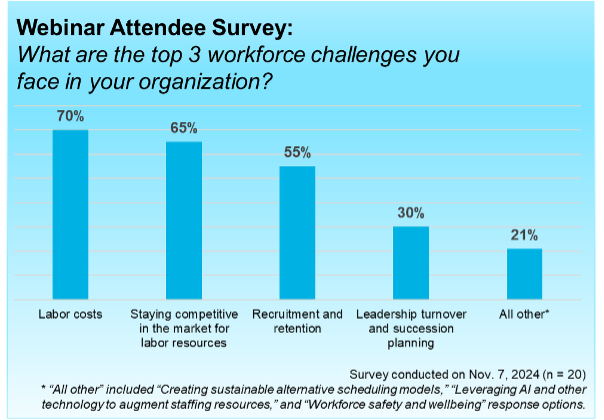
Hospital leaders attending the webinar were surveyed about their top three workforce-related challenges. Seventy percent of respondents said “labor costs,” followed by “staying competitive in the market for labor resources” (65 percent) and “recruitment and retention” (55 percent).
While shortages of nurses and many other clinical and non-clinical roles are projected to persist through the next several years, new strategic methods to manage workforce challenges are beginning to demonstrate return-on-investment. Previously unconventional approaches to labor pipeline management, employee retention, tech-enabled hiring processes and innovative scheduling models are poised for scale across hospitals and health systems of all sizes.
Keys to successful workforce management in 2025 include:
- Optimizing staffing models with attention to high-quality care.
- Leveraging workforce innovations and proven practices learned from industry leaders to fit an organization’s unique needs.
- Modernizing data analytics systems to demonstrate both return on investment and comparative performance to other organizations.
The webinar was sponsored by Premier’s Workforce Innovation Collaborative, a national collaboration among acute care hospitals that connects comparative operations data, clinical insights and proven practices to transform care delivery while managing costs.
Contact Thomas Flynn, Principal, Strategic Collaboratives, to learn how Premier’s Workforce Innovation Collaborative connects health systems to share and solve unique healthcare workforce challenges.
Learn More:
- See how Premier's advisory services team can help your organization unlock efficiency and improve outcomes with a Healthcare Rapid Assessment.
- Discover how Beebe Healthcare optimized its workforce and implemented sustainable operational changes with Premier as its partner.
- Take a deeper dive into Premier’s technology and advisory services that support workforce and performance improvement efforts.
I’m a healthcare improvement professional who designs, implements and provides leadership oversight for solutions that improve the quality, efficiency and cost of healthcare. I have a diverse blend of clinical, operational and analytical experience that spans pre-hospital, acute, chronic and long term care. When I’m not working, you’ll find me riding/racing bicycles through the woods or spending time with my son camping, snowboarding or nagging him to do chores.
Article Information
I’m a healthcare improvement professional who designs, implements and provides leadership oversight for solutions that improve the quality, efficiency and cost of healthcare. I have a diverse blend of clinical, operational and analytical experience that spans pre-hospital, acute, chronic and long term care. When I’m not working, you’ll find me riding/racing bicycles through the woods or spending time with my son camping, snowboarding or nagging him to do chores.