The End is Near: Are Providers Ready for the Unwinding of the COVID-19 Public Health Emergency?
The End is Near: Are Providers Ready for the Unwinding of the COVID-19 Public Health Emergency?
Key takeaways:
- A Premier survey of hospitals and non-acute providers reveals 69 percent of respondents are currently leveraging waivers or flexibilities granted by the Centers for Medicare & Medicaid Services (CMS) under the COVID-19 public health emergency (PHE) declaration.
- While roughly half of the organizations in the survey say 90 days or less provides sufficient notice to unwind the PHE waivers, the other half say they need at least 120 days’ notice.
- Using these insights as a barometer to ensure that patient care remains central to the goals of unwinding from the PHE, the Administration and Congress should work hand-in-glove with providers to ensure a smooth transition to pre-pandemic operations.
During the COVID-19 pandemic, health systems, non-acute care facilities and other providers relied on a host of regulatory flexibilities and waivers that are tied to the declaration of the COVID-19 Public Health Emergency (PHE).
Since January 2021, the U.S. Department of Health and Human Services (HHS) has promised at least 60-days' notice prior to ending the PHE to give states and healthcare providers a cushion to prepare. On Jan. 30, 2023, the White House announced it will end the COVID-19 PHE and national emergency declarations on May 11, 2023. By our count, HHS’ announcement provides 101 days advance notice.
On March 29, Congress passed a joint resolution that would immediately terminate the national emergency declared on March 13, 2020. President Biden has said that he will sign the legislation.
Premier’s Washington, D.C.-based Advocacy team recently canvased hospitals, health systems and other providers* to identify which waivers and flexibilities are still being leveraged and the readiness of providers to unwind from the PHE.
As a result, this development will not impact HHS COVID-19 operations, including regulatory waivers and flexibilities, and the May 11 expiration date for the PHE. The Centers for Medicare and Medicaid Services (CMS) has confirmed this interpretation via guidance posted on its website.
Premier canvased hospitals, health systems and other providers* to identify waivers and flexibilities being leveraged and the readiness of providers to unwind from the PHE.
Here’s what we found.
Ready or Not
Roughly half of responding organizations that are still using waivers felt 90 days was enough notice before the end of the PHE to allow them time to revert to pre-COVID-19 operations.
On top of that, among those respondents still using waivers, 80 percent said their organization already has a plan in place to unwind the waivers. These responses are encouraging, as they indicate that more health systems and providers are getting to critical mass when it comes to preparing for the retirement of the PHE regulatory environment. Furthermore, given the formal notification regarding the end of the PHE, these results provide reassurance that providers may be able to spring into action and begin unwinding swiftly.
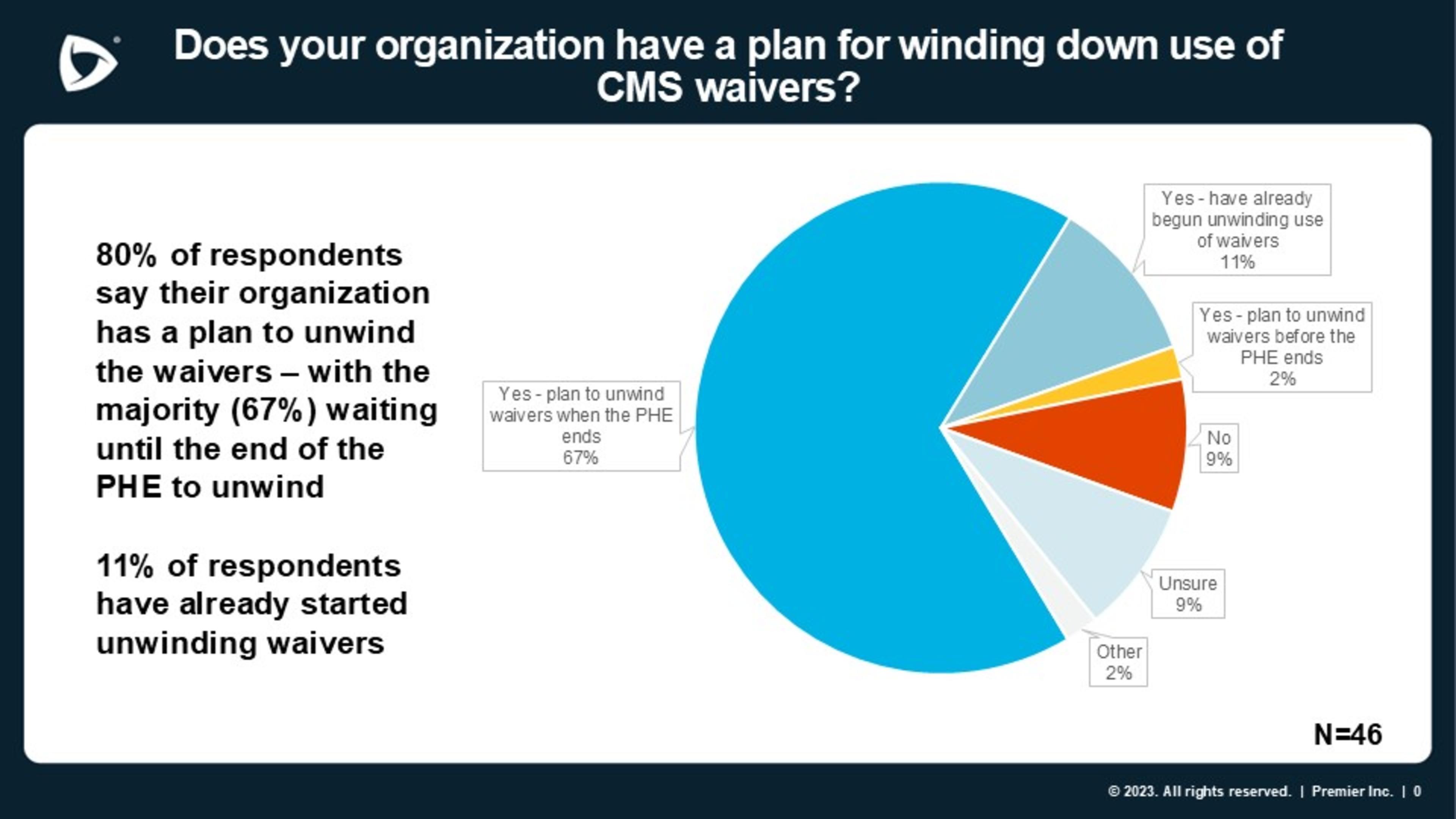
Source: Premier COVID-19 Waivers Wind Down Survey, January 2023
The other half of the story is equally, if not more, important. Slightly more than half of the organizations reporting that they are still using waivers and flexibilities said they need 120 days or more before they are equipped to do without them.
This tells us that healthcare providers will need the federal government to provide ample steppingstones in the form of resources, guidance and grace periods to help them in the journey back to normal operations. The Administration and Congress will need to work in lockstep with the provider community with multiple touch points along the way to ensure that patient care is not negatively impacted as the PHE declaration comes to a close.
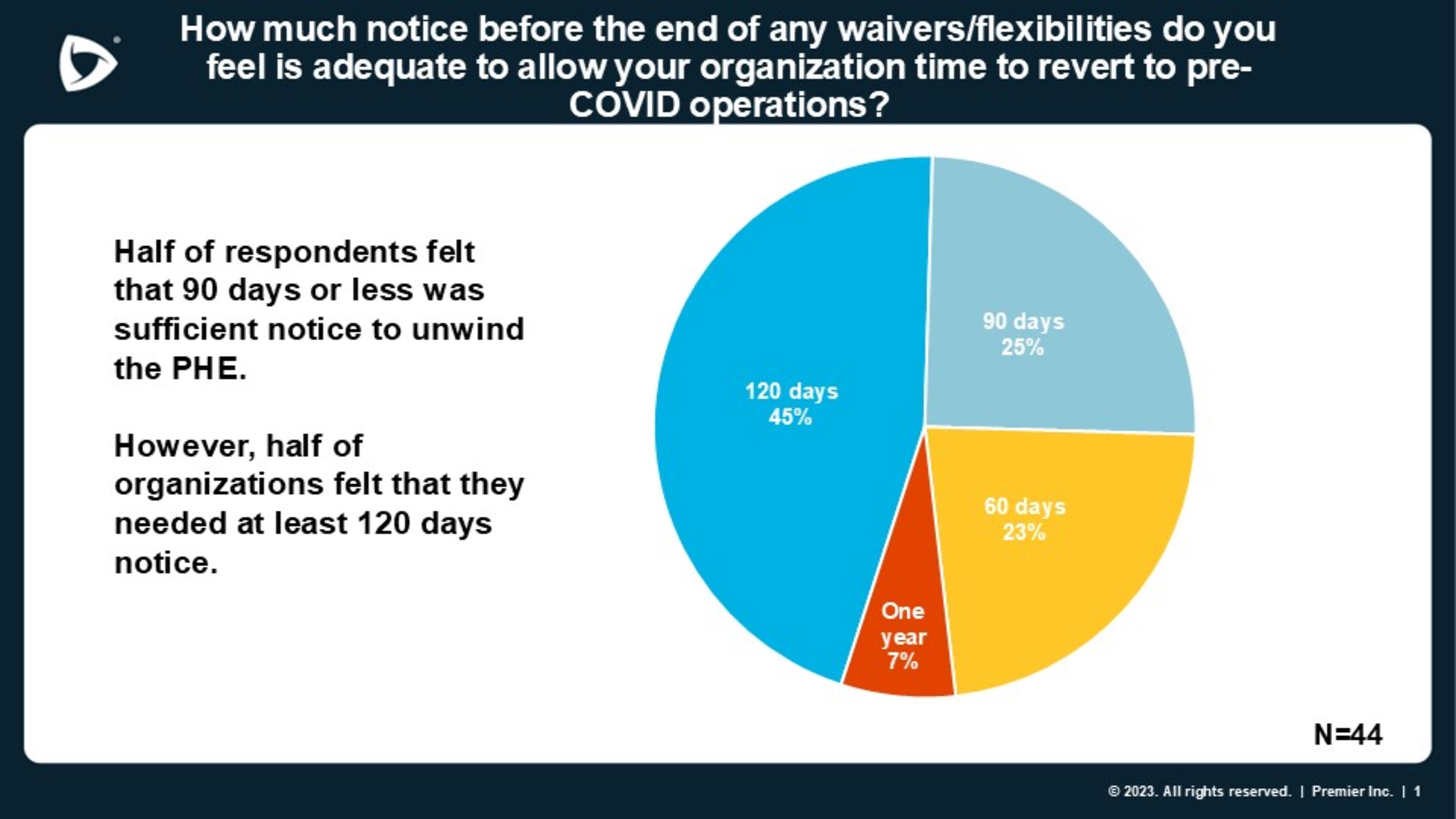
Source: Premier COVID-19 Waivers Wind Down Survey, January 2023
A Return to Business as Usual?
With a firm end to the PHE now in sight, healthcare providers face the daunting challenge of unraveling a broad array of regulatory changes that are now intertwined in many of their care practices and payment processes. In fact, roughly two-thirds of responding organizations are still utilizing COVID-19 waivers and flexibilities, according to Premier’s survey.
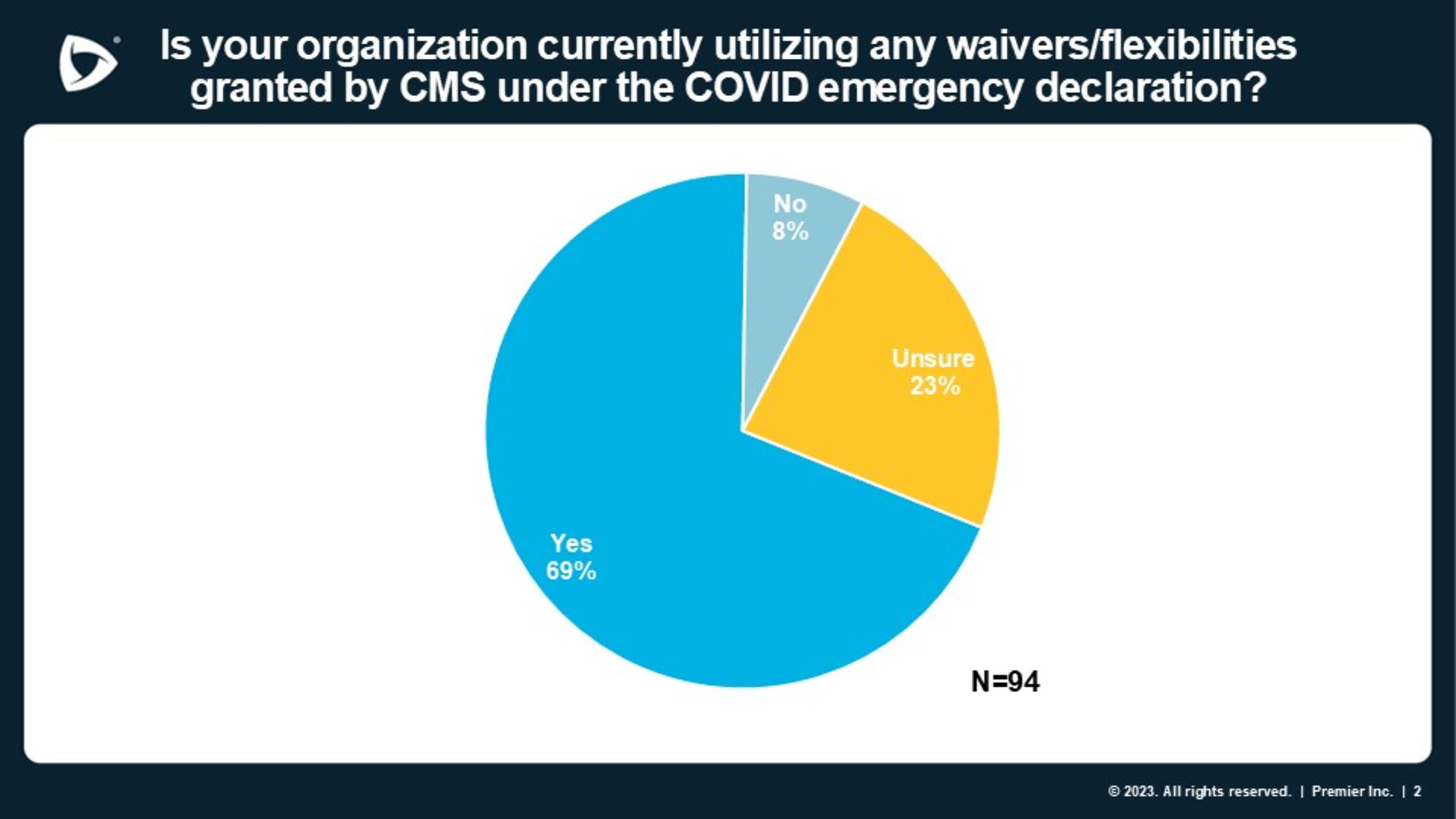
Source: Premier COVID-19 Waivers Wind Down Survey, January 2023
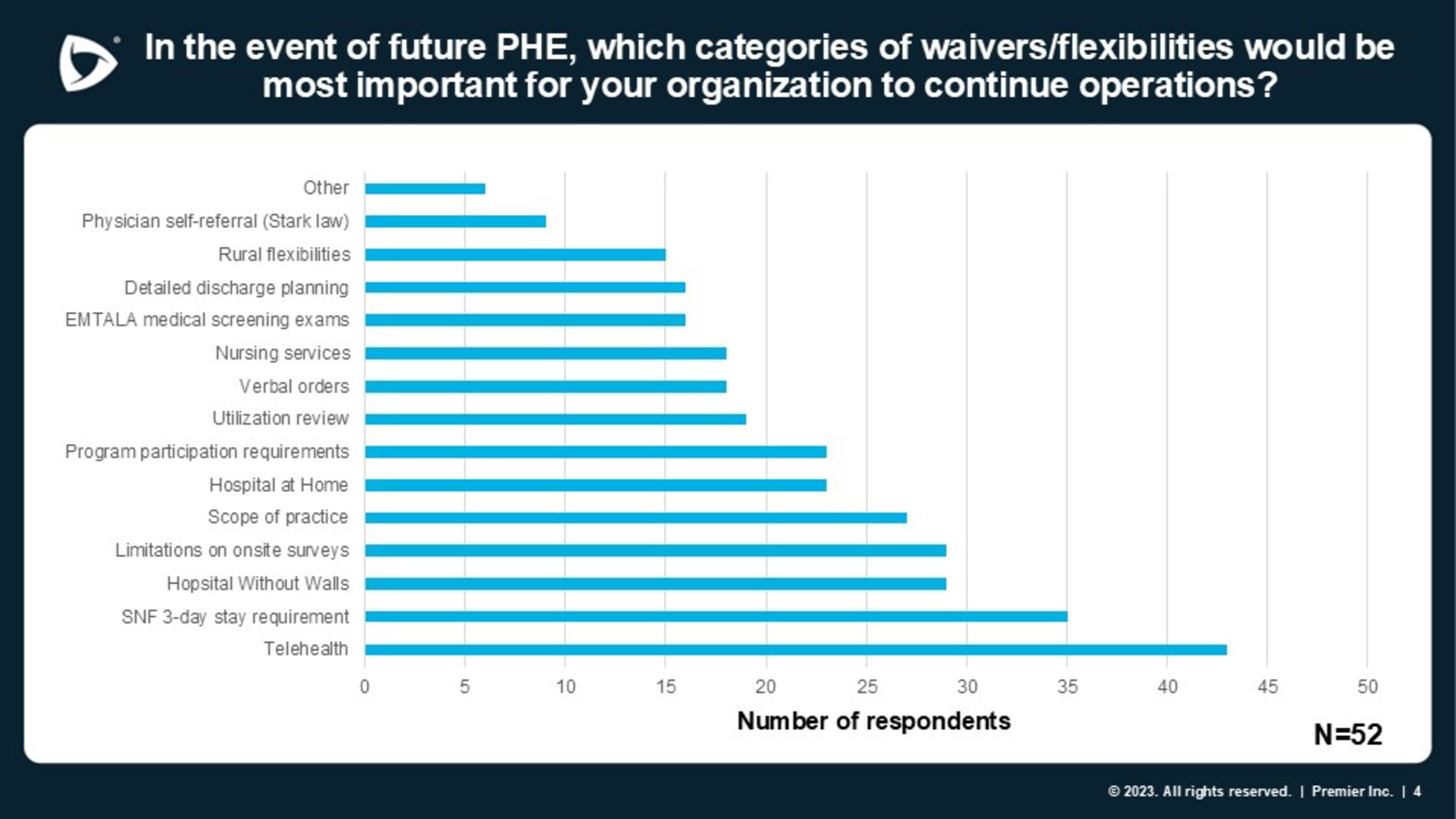
Not all waivers and flexibilities are created equal, and when asked which are most integral to their current operations, several emerged at the top, including expanded telehealth, waiver of the skilled nursing facility (SNF) three-day rule and flexibility regarding scope of practice.
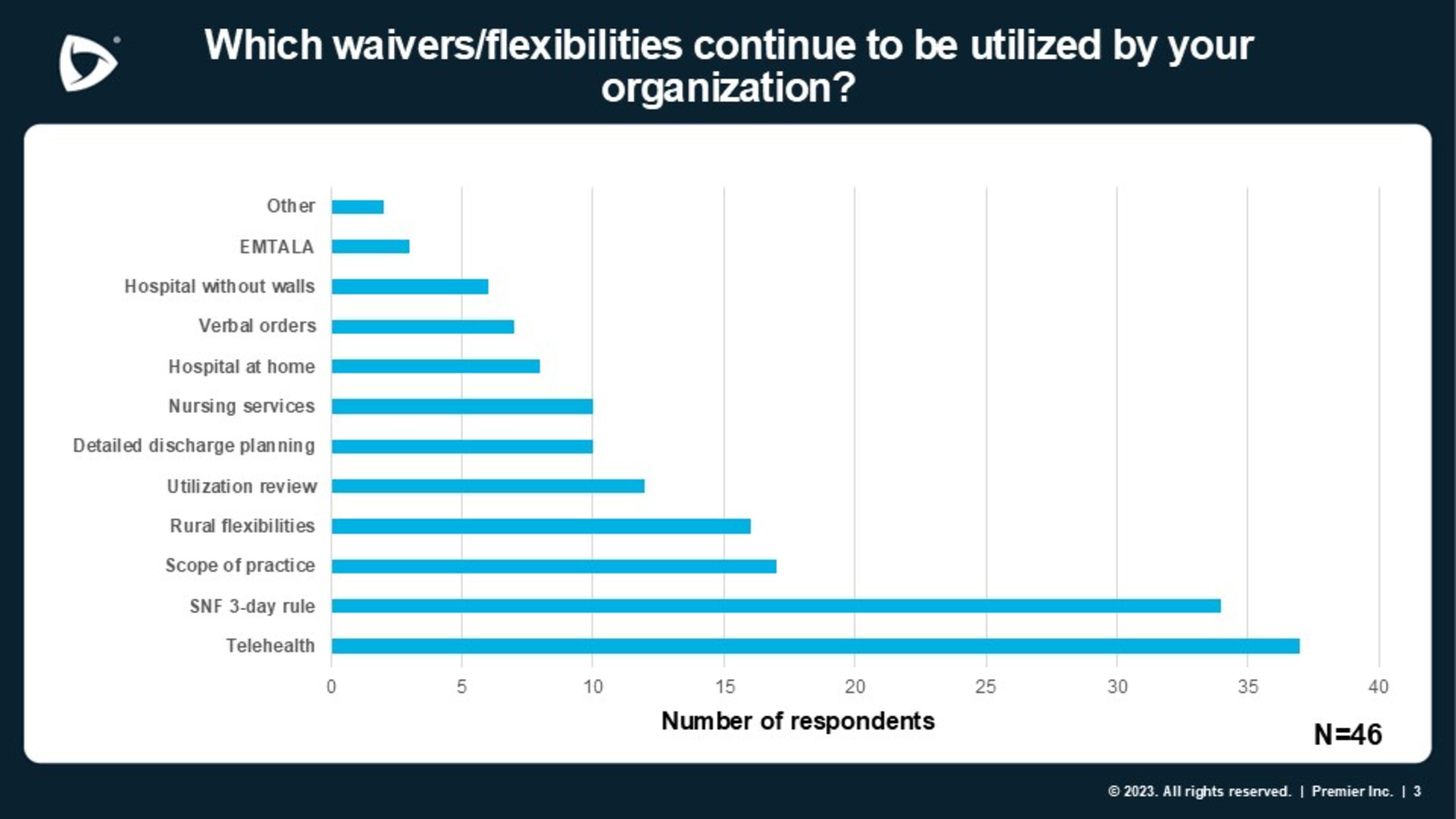
Source: Premier COVID-19 Waivers Wind Down Survey, January 2023
These closely align with the categories of waivers and flexibilities that organizations indicated would also be most important to continue operations in the event of future PHEs.
Source: Premier COVID-19 Waivers Wind Down Survey, January 2023
Telehealth: Telehealth has been a critical tool during the PHE, allowing providers to continue to furnish much-needed services to patients from the safety of their homes. The flexibilities CMS has granted around telehealth have served to highlight that many services can be effectively and efficiently furnished remotely. Congress recognized the value in easing barriers to virtual care and extended key telehealth flexibilities in the Consolidated Appropriations Act (CAA) of 2023 through the end of 2024, as advocated by Premier. The debate continues on making these flexibilities permanent.
Additionally, while several telehealth policies were extended in the CAA, there are other related flexibilities not included and it will be critical for CMS and other agencies to clarify for providers which policies will conclude with the end of the PHE. For example, many hospitals were able to furnish services outside the walls of their facilities using telehealth or virtual care under the Hospitals without Walls initiative.
Another telehealth-related flexibility not extended in the CAA is a waiver granted by the Drug Enforcement Agency (DEA) that allows practitioners to prescribe controlled substances to treat opioid use disorders (OUDs) without having to interact in-person with their patients. A recent Premier analysis revealed the tremendous cost of caring for patients with OUDs in the hospital setting and the significant disparities that exist among those diagnosed with OUD.
The DEA recently proposed new regulations that would make permanent some of the flexibility to prescribe remotely. While Premier generally supports the agency’s efforts to increase access to certain controlled substances, Premier expressed concern in comments that the agency’s approach is too restrictive and fails to build on lessons learned during the pandemic, the positive results documented on patient access and outcomes, and the work of other agencies in this area.
Hospital at home: More than 200 hospitals across 34 states –including many health systems in the Premier alliance –have embraced the “hospital at home” concept and have tailored their programs to effectively provide acute care for patients in the comfort of their own homes. This new avenue of care has freed up hospital capacity, offered a safe and effective method to care for patients and reduced avoidable emergency department visits.
There is good news in the CAA of 2023 on this account as well. Congress used this legislative vehicle to extend the CMS Acute Hospital Care at Home (AHCAH) waiver for two years. Looking further down the road, opportunity exists to develop policies to allow for the continuation and growth of the hospital at home concept, including addressing existing challenges and ensuring a sustainable ongoing program.
SNF three-day rule: CMS has waived the requirement that Medicare beneficiaries have a three-day hospitalization to be eligible for skilled nursing facility (SNF) services under the PHE.Waiving the three-day stay requirement can help avoid inappropriately lengthening inpatient stays when a patient can safely be discharged earlier to a lower cost of care setting. The SNF waiver has been relied on to free up hospital beds and relieve overwhelmed acute care facilities during the pandemic.
Healthcare labor scope of practice: As part of the PHE, CMS waived several requirements related to scope of practice to ensure providers can fully maximize their workforce. For example, CMS waived requirements that a certified registered nurse anesthetist be under the supervision of a physician. These waivers had the effect of deferring to state laws and requirements related to supervision and licensure.
While Congress adopted Premier-supported recommendations in the CAA 2023 to expand the number of physicians in the training pipeline by increasing future residency slots for the Medicare graduate medical education (GME) program, shortages will remain a problem in the short term. Given persistent workforce shortages and staff burnout, organizations are seeking extended flexibilities to deal with these challenges.
Organizations also called out other actions that CMS could take to help them plan for winding down waivers from the PHE, including greater coordination by the federal government in dealing with conflicts between federal and state waivers.
The Stakes are High, Premier is Stepping Up
Over the past three years, Premier has joined other provider organizations in asking HHS to renew the COVID-19 PHE to ensure the continuation of important waivers, flexibilities and enhanced Medicaid funding as the pandemic persisted. In anticipation of the inevitable end to the PHE, Premier also provided HHS with recommendations on how it should use its authority to maintain or expand important waivers.
As the Administration and Congress weigh how to unwind the COVID-19 PHE, a data-driven approach to complex decisions such as this is integral. Premier’s hope is that these insights, direct from healthcare providers, will inform the federal government’s approach. Given the limitations* of Premier’s survey, we encourage HHS to conduct a more rigorous and expansive assessment of the nation’s readiness to close out the PHE and work closely with the provider community to ensure patient care is not negatively impacted.
For those areas where the Administration does not have regulatory authority, Congress should consider legislation to create targeted policies that will allow important care transformations that have emerged out of the pandemic to continue uninterrupted. As part of this, Congress should also keep an eye towards flexibilities that help address staffing and other healthcare challenges that do not end just because the PHE does.
The bottom line: Knowing when the PHE will end provides a welcome goalpost that providers can begin to plan for. However, simply putting an end date and FAQ documents forward is not enough to ensure a smooth transition to pre-COVID operations. Providers will need resources, clarifying guidance and more to successfully adjust to the new normal and ensure continuity in patient care, especially in an environment where providers are plagued by financial distress and labor challenges.
*Survey Methodology
Premier canvassed healthcare stakeholders from Jan. 22-30, 2023, on a number of topics related to COVID-19 waivers and flexibilities to help inform policymakers as they look to unwind the PHE. Approximately 94 individuals responded, representing a range of small to large health systems and non-acute care providers and at least 324 acute care facilities and more than 860 non-acute providers. Not every respondent answered every question. Approximately 69 percent of respondents reported that their organization is currently utilizing waivers and flexibilities granted under the COVID-19 PHE.
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.

Melissa supports healthcare stakeholders on policies related to provider reimbursement and alternative payment models. She previously served in the Federal government and is experienced in analyzing and formulating recommendations on Medicare payment policies and Innovation Center models.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.

Melissa supports healthcare stakeholders on policies related to provider reimbursement and alternative payment models. She previously served in the Federal government and is experienced in analyzing and formulating recommendations on Medicare payment policies and Innovation Center models.