The Secret Ingredient in Post-COVID-19 Margin Improvement

In a time of rapidly changing markets, the COVID-19 pandemic has exacerbated healthcare providers’ margin pressures. One estimate shows hospitals losing about $1,200 per COVID-19 case. While providers received some help in the form of $100 billion of emergency relief fund in the Coronavirus Aid, Relief, and Economic Security (CARES) Act, hospitals will need to take action in order to compensate for falling revenues and changing cost structures.
To stimulate swift margin improvement, hospitals and health systems must assess the cost implications of COVID-19, and should use their assessment to develop a realistic and actionable financial transformation strategy that enhances revenue while reducing expenses.
Macro vs. Micro: Conducting a COVID-19 Situational Analysis
To understand the current financial position, as dictated by COVID-19, providers should consider both revenue and expense drivers. Understanding the macro trends is the first step. Broadly, the most recent labor numbers indicate a national unemployment rate of nearly 15 percent. Providers will need to work with their local economic partners to understand how their geography has been impacted. Changes in patient mix will undoubtedly trickle down to cost-side implications, as many patients who previously had commercial insurance may now fall into the uninsured bucket.
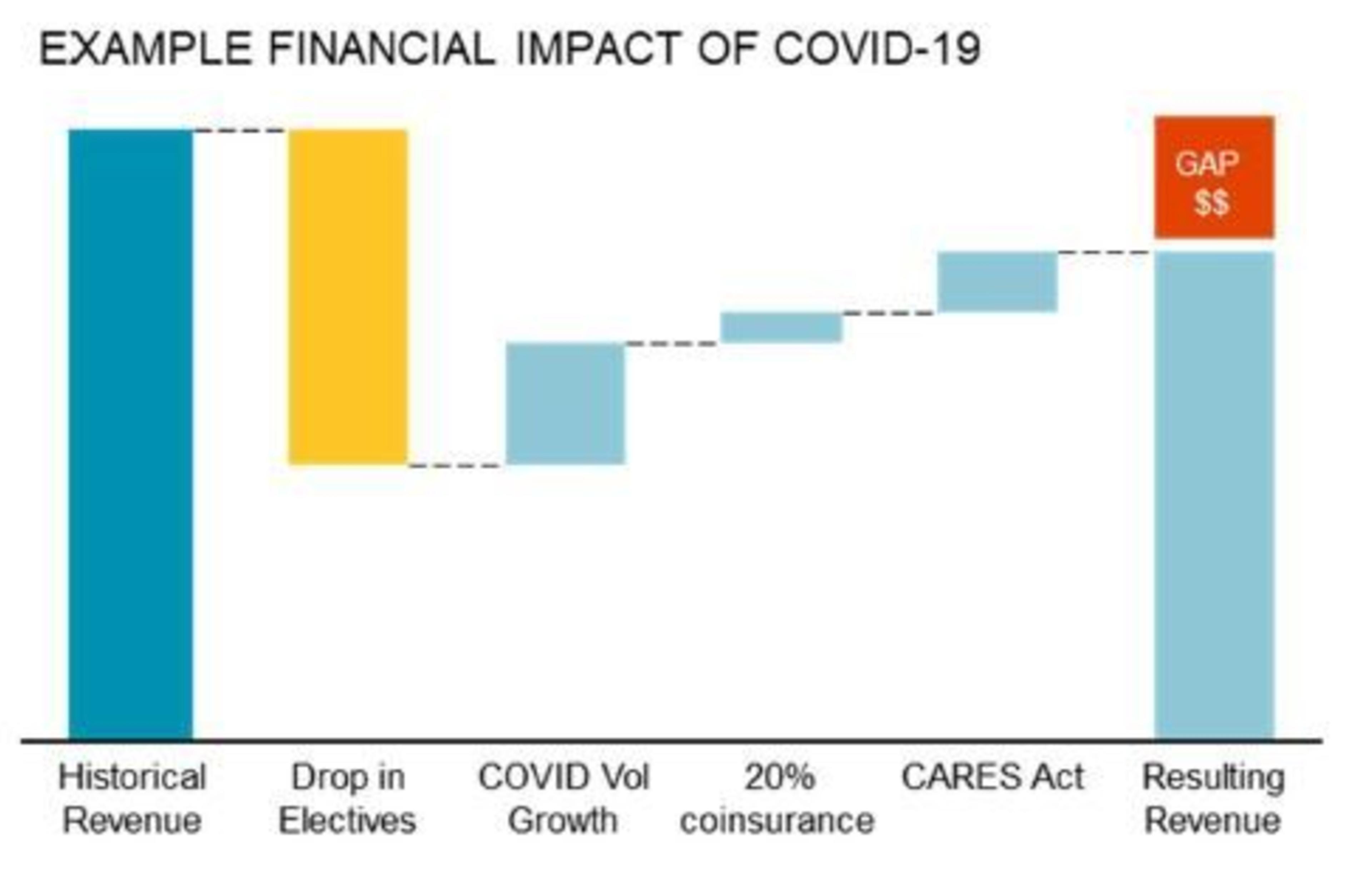
A strong situational analysis will also require providers to dive a level deeper into their current state at a micro level. The clearest impacts to the bottom line emerge when looking at facility revenue. Thirty states plus the District of Columbia issued limitations on elective and non-emergent surgical cases as the pandemic picked up. While some are now considering resuming elective surgeries, these procedures are a large revenue driver for many providers, and losing two to three months of elective cases has the potential to create an insurmountable deficit.
In addition, COVID-19 has encouraged potential patients to delay seeking care, even for issues as critical as heart attacks, creating another financial challenge for providers. While the CARES Act provides some revenue relief, for many providers it’s just the tip of the iceberg.
On the other side of the equation, providers must consider the expenses associated with the COVID-19 crisis. The Centers for Disease Control reports that the median intensive care unit (ICU) stay for a COVID-19 patient is 10 to 13 days, compared to the average hospital length of stay of 4.6 days. Further, an analysis by Johns Hopkins University Center for Health Security estimates that treating a COVID-19 patient in the ICU requires 340 gloves per day.
This cost increase is slightly offset by cost decreases associated with variable expenses from elective procedures, while overhead like labor, capital and administrative costs are largely holding steady. COVID-19 patients are driving some revenue, but at a higher cost, creating a challenging situation for already financially stressed providers.
The Secret Ingredient: A Force Multiplier
A force multiplier is a factor that allows organizations to accomplish greater feats than without it. When providers understand how to wield a force multiplier in the context of their post-COVID rapid cycle margin improvement, their revenue recovery efforts can be exponentially accelerated, allowing them to return to financial, operational and clinical health sooner.
As a purpose-built company, Premier works with hospitals, health systems and other providers to harness existing technologies, buoyed by a database that captures powerful insights on 45 percent of discharges nationally, to collaboratively create an improvement plan. This approach empowers providers to take a holistic view of their current situation and move quickly to support – and accelerate – the health of their organization.
Operational Stabilization
While there are countless areas for analysis in the provider ecosystem, focusing on five key areas grounds the understanding of current state, resources available and strategic advantages that can drive improvement:
- Balance sheet/cash flow
- Programmatic rationalization
- Corporate/fixed costs
- Revenue cycle
- Reactivation
By staying focused on these fundamental areas, providers can leverage technology-enabled, clinically integrated solutions to work quickly and arrive at operational stabilization sooner. Using the force multiplier lens on these five key areas allows providers to not only understand the current state, but recognize the changes that must be made in both the short and long term to ensure sustainable transformation.

Doing nothing is simply not an option.
Providers across the country are facing increased costs, shrinking revenues and the charge to provide high-quality care for their community members amid a global pandemic. More than ever, providers need the capability to identify the root cause of their systemic problems and create technology-enabled, clinically integrated solutions to fix them.
With the right collaboration, it’s possible to go beyond a quick fix and hardwire transformative, sustainable results. And with the right technology, expertise and partners, providers will be enabled to more quickly succeed with their reactivations post-COVID and beyond.
Better, stronger, faster – why go it alone? Contact us to learn how Premier can help enable your rapid-cycle margin improvement.
Roger has more than 20 years of experience leading healthcare transformation through innovative partnerships between health system providers, medical device companies and consulting firms.
Paul has a track record of delivering financial results for clients across the healthcare value chain including providers, biotechnology firms and device companies. Areas of expertise include strategic partnership contract structuring, ancillary and clinical department operations, and supply chain process standardization.
Article Information
Roger has more than 20 years of experience leading healthcare transformation through innovative partnerships between health system providers, medical device companies and consulting firms.
Paul has a track record of delivering financial results for clients across the healthcare value chain including providers, biotechnology firms and device companies. Areas of expertise include strategic partnership contract structuring, ancillary and clinical department operations, and supply chain process standardization.