Trend Alert: Private Payers Retain Profits by Refusing or Delaying Legitimate Medical Claims
Key Takeaways:
- Nearly 15 percent of all claims submitted to private payers for reimbursement are initially denied, including many that were pre-approved to move forward through the prior authorization process.
- Denied claims tended to be more prevalent for higher-cost treatments, with the average denial pegged to charges of $14,000 and up.
- Over half (54.3%) of denials by private payers were ultimately overturned and the claims paid, but only after multiple, costly rounds of provider appeals.
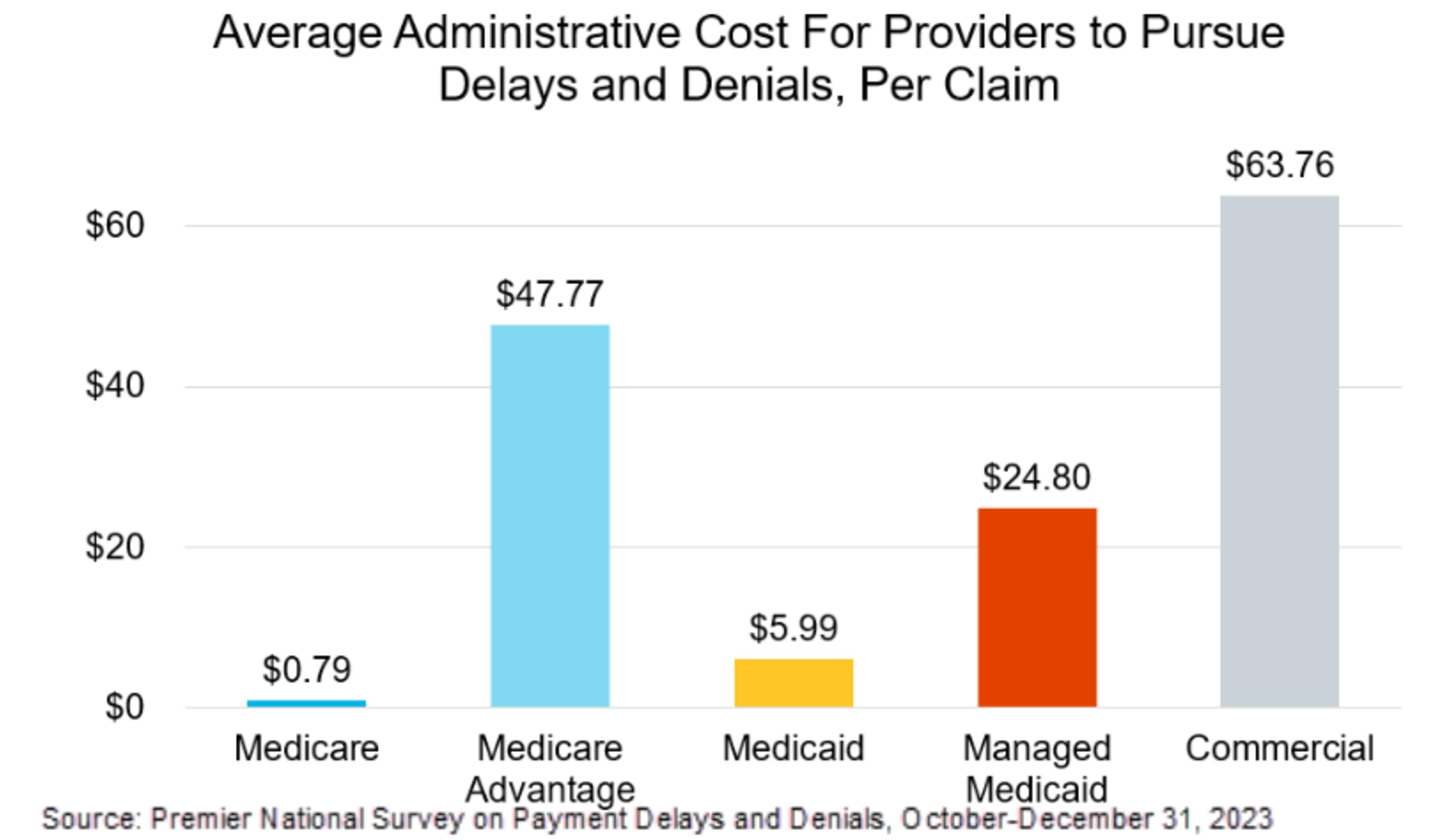
- The average cost incurred by providers fighting denials is $43.84 per claim – meaning that providers spend $19.7 billion a year just to adjudicate with payers.
Premier and 118 member organizations sent a letter to the Centers for Medicare & Medicaid Services (CMS), highlighting the results of the below survey and providing CMS recommendations to address payment denials and delays in Medicare Advantage.
Nearly 15 percent of medical claims submitted to private payers for reimbursement are initially denied, according to a new national survey of hospitals, health systems and post-acute care providers conducted by Premier, Inc. An average of 3.2 percent of all claims denied included those that were pre-approved via the prior authorization process.

Despite the initial denial, more than 54 percent of claims rejected by private payers were ultimately paid. Many others may have been ultimately paid but were not fully pursued for payment due to issues such as resource constraints.

Denials tended to be more prevalent for higher-cost treatments, with the average denial pegged to charges of $14,000 and up.

Unnecessary Insurer Denials Add Costs to the System and Compromise Hospital Financials
Hospital and health system respondents that fought the denials did so at an average cost of $43.84 per claim. Considering that health insurers process about three billion medical claims each year, this means that providers spend about $19.7 billion a year in these reviews, more than half of which ($10.6 billion) was wasted arguing over claims that should have been paid at the time of submission (see Methodology section for more detail).
Importantly, this figure does not include the costs associated with added clinical labor, which the American Medical Association estimates adds $13.29 to the adjudication cost per claim for a general inpatient stay and $51.20 to the cost of inpatient surgery.
There are indirect costs to denials as well. To get from denial to ultimate payment, Premier survey respondents reported that they needed to conduct an average of three rounds of reviews with insurers, with each review cycle taking between 45 and 60 days. These delays resulted in nearly 14 percent (13.9) of all health system claims being past due for remittance, with providers often unable to recoup costs for up to six months after services were delivered.

This continued burden has a tremendous impact on hospitals' financial viability. Over the past year, the average days of cash on hand for hospitals and health systems declined by 44 days over the previous year, on average - a 17 percent drop year over year. Lacking cash on hand, health systems are unable to re-invest in patient care and may also suffer from downgrades in bond ratings, making cash more expensive and harder to obtain. In contrast, days of cash on hand increased for insurers like United Health Group (up 25.5 percent on average from 2019) and Cigna (up 24.4 percent on average from 2019).
Denials Are Also Costly for Patients
Patients whose bills are unpaid by their insurer may be liable for some or all of the ultimate costs of care.
According to The Commonwealth Fund, 46 percent of Americans say they skip or delay necessary follow-up care because they are worried about the costs and another 49 percent say they would be unable to pay for an unexpected $1,000 medical bill within 30 days. A lengthy period of limbo may, therefore, result in patients delaying necessary follow-up care until they can be certain that existing hospital bills will be paid.
Looking specifically at the Premier survey data, respondents reported that hospital discharges to post-acute care settings such as skilled nursing facilities (SNF) were particularly subject to initial denials, with more than 20 percent of all claims requesting discharge to a SNF for ongoing care and post-acute therapy denied by private insurers.

The net result of these denials is longer than expected hospital stays, which adds expense and risk, as patients with longer stays have greater rates of secondary infections, falls and exposure to other contagious diseases. Moreover, payer denials have downstream effects on care availability, as patients requiring a hospital admission may not have access to a bed until other patients are approved for discharge to the SNF setting of care.
Downstream Impact of Denials on Quality Ratings and Reimbursement
According to research, patients subjected to claims denials rated their satisfaction with delivered care 8.2 points lower than those without denials, as assessed by the 100-point scale in the Consumer Assessment of Healthcare Providers and Systems (CAHPS) survey. This finding held true even when the claim was ultimately paid.
With a 15 percent overall rate of denials, as found in the Premier survey, providers’ overall quality measures scores are being artificially depressed by payer actions.
Poor quality scores have a host of financial impacts. For health systems with practitioners participating in alternative payment models (APMs) that tie payments to performance, lower quality scores curb their ability to earn upside bonus payments and may even lead to payment penalties. Quality metrics are also evaluated by payers, who factor quality scores into the overall rates they are willing to pay for services, reserving the best payment rates for the best performers. In this way, payers have a perverse incentive to increase denials, as it ultimately leads to poorer quality scores and lower overall reimbursement rates – not to mention increased profits for themselves.
The Path Forward
Premier and our members have significant concerns about the potential impact of payment delays and denials on patients’ access to healthcare, and we continue to work with Congress and the Biden Administration to remove barriers to high-quality, equitable care.
One area of concern is the Medicare Advantage (MA) program, where over a quarter of claims are subject to prior authorization, and nearly 20 percent of discharges to post-acute care settings are initially denied. Policy levers to address these issues include:
- Premier continues to urge CMS to stringently monitor reporting of expenditures on direct patient care, particularly in the MA program. Premier also encourages CMS to begin collecting data on payment delays and denials between MA plans and contracted providers to determine whether the practice violates CMS’ expectations around network adequacy. While MA plans may claim a contracted network of providers on paper, adequate payment to these networks is critical to continued access to care for Medicare beneficiaries. Premier will continue to work with Congress to help ensure CMS has the statutory authority needed to enforce its regulations, including urging Congress to hold oversight hearings to combat bad actors in this space. Premier applauds CMS’ recent regulatory changes to streamline prior authorization requirements in the MA program, including prohibiting the use of prior authorization for Medicare beneficiaries who may switch health plans during an active course of medical treatment. It is imperative that CMS work expeditiously to enforce these requirements to protect patients’ continuity of care. Additionally, when MA plans do utilize prior authorization as a tool for medical management, coverage determination reviews should be conducted by physicians of the same specialty for the service being reviewed – not a cost-containment algorithm.
- As policymakers consider requirements for MA plans to utilize electronic prior authorization, Premier encourages going a step further to stipulate that claims approved under an electronic prior authorization may not be artificially delayed or denied. In essence, electronic prior authorization should serve as an agreement between the payer and provider to perform the requested service and remit timely payment for it. It is critical that federal regulators leverage the technology pathways that already exist to streamline prior authorization as soon as possible, rather than waiting years for health plans to catch up.
- CMS has moved away from holding MA plans accountable for CAHPS and other patient experience measures in recent rulemaking. Premier continues to recommend that CMS return to its past policy of weighting patient experience and access measures more heavily in the MA Star Ratings methodology, empowering beneficiaries to hold their health plans financially accountable.
- Premier urges CMS to take enforcement action against MA plans that fail to abide by the coverage rules of Medicare, which has included coverage of post-acute skilled nursing services since Congress created the Medicare program in 1965.
Methodology
Premier conducted a voluntary, national survey of member hospitals and health systems from October 10-December 31, 2023. Respondents represented 516 hospitals across 36 states, accounting for 52,123 acute care beds. Respondents were asked to consider all claims from January 1, 2022 to December 31, 2022. Findings are presented as averages, weighted by acute bed capacity of the respondent. Respondents ranged from a small 12-bed critical access hospital to large, multi-state health systems. A copy of the survey questions can be found here.
To calculate the costs associated with fighting payer denials, we multiplied the 3 billion claims processed each year by 0.15 (the average denial rate identified by the survey) to determine that 450 million claims were subjected to denials. We then multiplied that figure by $43.84 (the average cost incurred) to calculate $19.7 billion in costs. Considering that 54.3 percent of these claims were ultimately paid, we multiplied $19.7 billion by 54.3 percent to calculate the costs that were largely unnecessary.
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.

Mike is focused on driving innovation in healthcare and leading the industry through transformation by co-developing solutions with key stakeholders to help healthcare providers deliver higher quality care at a better cost.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.

Mason leads Premier’s policy development on issues related to Medicare Advantage and private insurance markets. He leverages his insurance industry expertise to support Premier’s members in the multi-payer movement to value.
Article Information

Mike is focused on driving innovation in healthcare and leading the industry through transformation by co-developing solutions with key stakeholders to help healthcare providers deliver higher quality care at a better cost.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.

Mason leads Premier’s policy development on issues related to Medicare Advantage and private insurance markets. He leverages his insurance industry expertise to support Premier’s members in the multi-payer movement to value.