Health Systems Report that Policy Changes are Needed to Accelerate Adoption of Risk-Based Payment Arrangements

Hospital and health system leaders reveal that movement to risk-based payment models is moving slowly, most claiming that less than 20 percent of their patient population is covered under such arrangements, according to a recent Premier healthcare alliance survey. These healthcare providers remain interested, however, in greater engagement in risk-based payment models ranking Medicare Advantage, employer-sponsored health plans and fee-for-service Medicare as the three priority areas.
Risk-based models include accountable care organizations (ACOs), bundled payments, and other types of alternative payment models (APMs) that hold providers accountable for the cost and quality of care across the continuum. The survey also revealed the fundamental reasons for this slow pace, which largely amounts to needed economic incentives and access to timely and accurate claims data. This points to needed policy changes, as well as action by private organizations.
Results from the survey illustrate how the transition to risk-based models has been slow and market dependent
Across all payer types, most respondents indicate that less than 20 percent of their population was covered in a risk-based arrangement.
- Less than 20 percent of respondents reported having more than half of their population covered by Medicare fee-for-service risk-based arrangements.
- 55 percent cited less than 20 percent of their Medicaid population was covered by a risk-based arrangement.
- 60 percent said less than 20 percent of their Medicare Advantage patient population is covered by risk-based arrangements.
- 64 percent of respondents reported that less than 20 percent of their patient population was covered by risk-based arrangements with employer-sponsored health plans.
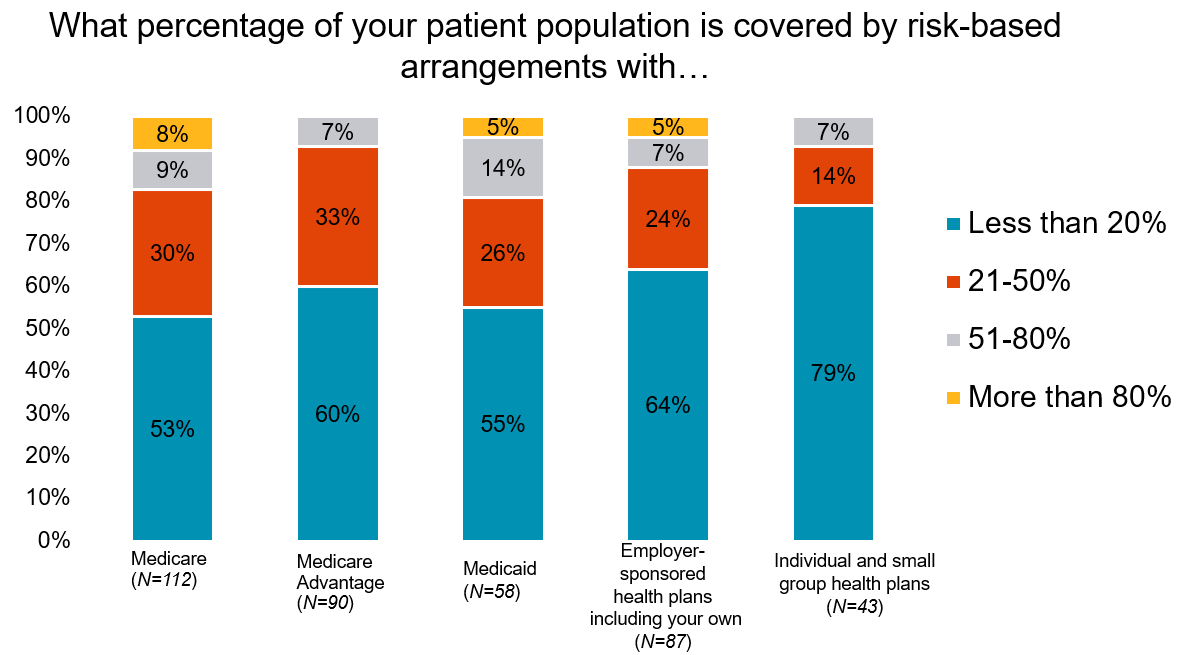
Over the next five years, only 5 percent of respondents expect to have more than 80 percent of their population in risk-based arrangements.
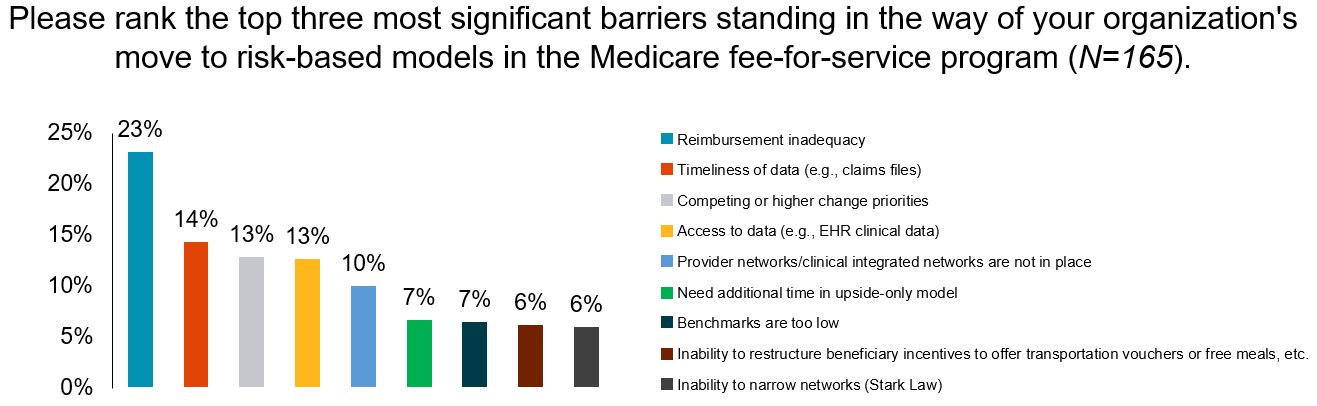
The survey revealed the top barriers standing in the way of organizations moving to risk-based models in the Medicare fee-for-service program
Reimbursement inadequacy was ranked the top barrier standing in the way of shifting to risk-based models in the Medicare fee-for-service program.
The survey revealed that providers need more access to timely, accurate and complete claims data as the shift to risk-based models unfolds.
- Timeliness of data was ranked as the second most significant barrier and access to data was tied for third.
- Gaining access to commercial claims data is a particular challenge for hospitals and health systems.
- 20 percent of respondents said they do not get data from commercial payers
- Only 3 percent said that the data they do receive is both accurate and standardized.
Congress can address these barriers to ease the transition to risk-based arrangements
Congress can recognize the upfront investment needed by healthcare providers to move to two-sided risk by:
- Extending the 5 percent payment bonus that Congress created in the Medicare Access and CHIP Reauthorization Act (MACRA) for providers who participate in an Advanced APMs;
- Improving cost performance benchmarks so that providers who are achieving savings every year are not negatively impacting their own benchmark; and
- Restoring to at least 50 percent the rate of savings that Medicare shares with providers participating in total cost of care models.
Providers need greater flexibility to innovate and coordinate care, including:
- Changes to the Stark physician self-referral and antikickback laws to reflect the shift to models that hold providers accountable for quality and cost.
- Being allowed to tailor benefits to incentivize care, much like is done in Medicare Advantage.
Congress can also require federal and commercial payers to provide timely access to administrative and claims data to healthcare providers, especially those in value-based care arrangements.
What's being said?
"Strong partnerships between payers and providers are key to moving to risk-based contracts that will transform the way care is delivered and drive better outcomes and value. These partnerships need to be built on access to standardized claims data, shared risk, clarity of roles and responsibilities and transparent business relationships." - Carrie Nelson, MD, Chief Clinical Officer of Advocate Physician Partners
"There is a great deal of uncertainty as we explore moving to risk-based contracts. We call on the Administration to provide more details on the emerging alternative payment models to help inform the best path forward for our system." - Steve Neorr, Senior Vice President and Chief Administrative Officer, Triad HealthCare Network.