New CMS Transforming Episode Accountability Model (TEAM): What Providers Need to Know

Key Takeaways:
- Launching January 1, 2026, TEAM requires selected acute care hospitals to coordinate care for traditional Medicare beneficiaries undergoing one of the surgical procedures included in the model.
- To succeed in the program, participants must develop effective care pathways and protocols as well as have a strong provider engagement strategy.
- Premier offers a wide range of expertise in TEAM and bundled payment model readiness, preparation, development and implementation.
After years of hinting that a mandatory bundled payment model was imminent, in August 2024 the Centers for Medicare & Medicaid Services (CMS) finalized the Transforming Episode Accountability Model (TEAM). TEAM is a key facet of CMS’ strategy to support person-centered, value-based specialty care, which was released in late 2022.
TEAM will launch on January 1, 2026, and run for five years, ending on December 31, 2030. The model’s goal is to support people with Medicare undergoing certain surgical procedures by aiming to promote better care coordination, seamless transitions between providers and successful outcomes.
Here we delve into the critical features of the mandatory TEAM model and its potential implications for healthcare providers.
What is the CMS Transforming Episode Accountability Model (TEAM)?
The mandatory, episode-based payment model is broad and far-reaching. Selected acute care hospitals will coordinate care for traditional Medicare beneficiaries undergoing one of the surgical procedures included in the model (i.e., initiate an episode).
In year one, CMS proposes that TEAM focus on five specific procedural episodes:
- Lower extremity joint replacement
- Surgical hip femur fracture treatment
- Spinal fusion
- Coronary artery bypass graft
- Major bowel procedure
TEAM will concentrate on payments for a defined episode of care, linking payments for all items and services provided during the initiating procedure, plus a 30-day post-discharge window, inclusive of inpatient and outpatient services. The model also includes a risk-sharing component, holding providers accountable for the quality and total cost of care during the episode.

What are the Implications of TEAM?
TEAM is a mandatory program, unlike Bundled Payment for Care Improvement-Advanced (BPCIA), which is voluntary. TEAM will require selected hospitals to coordinate patient care and engage with specialists to enhance quality and reduce costs.
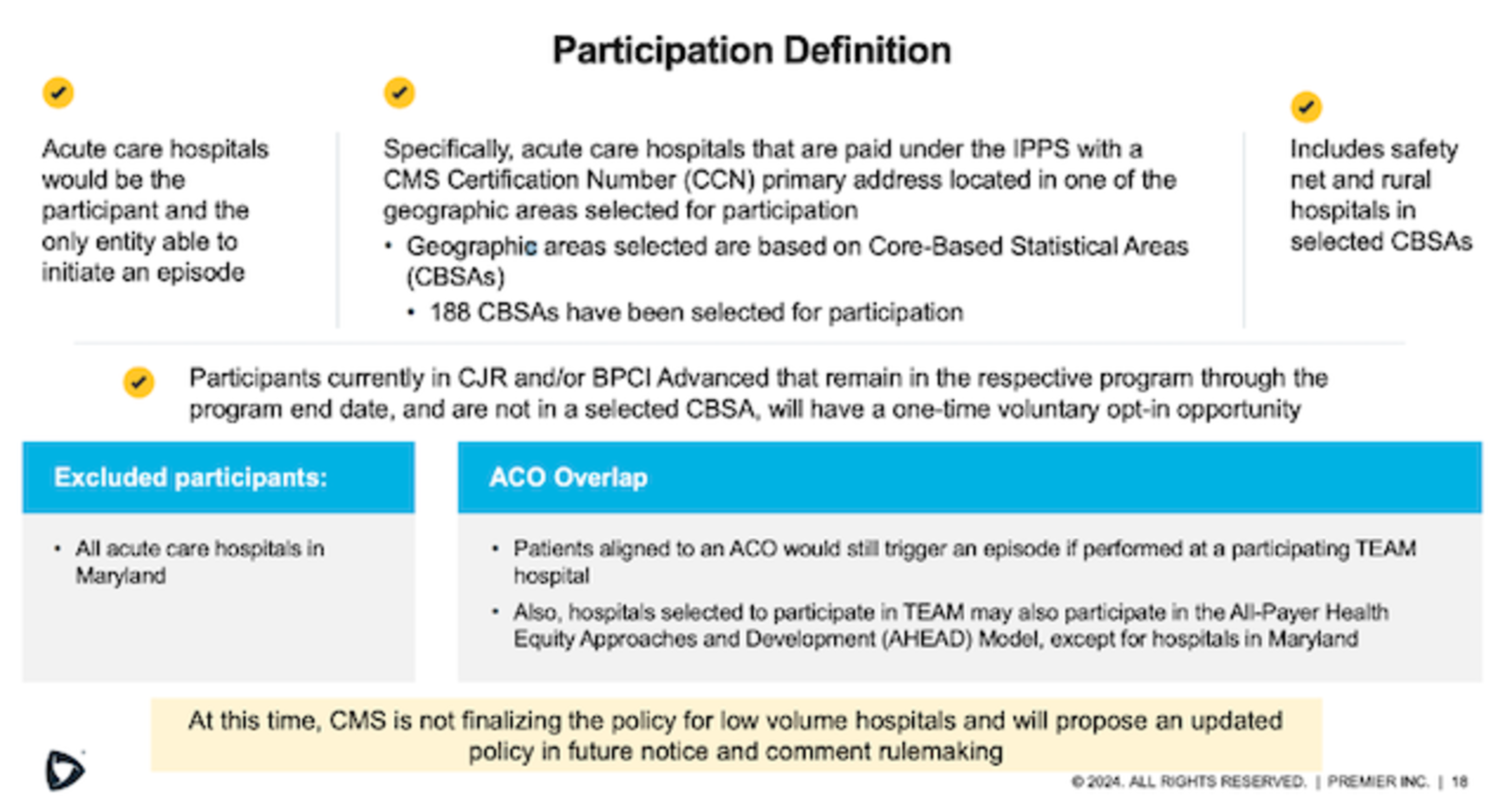
TEAM participation will be based on geographic areas using core-based statistical areas (CBSAs).
- CMS has stratified CBSAs into groups based on average historical episode spending, number of hospitals, number of safety net hospitals and the CBSA’s experience in prior CMS bundled payment models.
- All acute care hospitals in Maryland are excluded as eligible CBSAs for selection in TEAM, as are CBSAs where hospitals generated no episodes in any of the five-episode categories between January 1, 2022 – June 30, 2023.
- 188 CBSAs have been selected for TEAM participation.
Accountability for surgical episodes, including the period following surgery, encourages hospitals to work closely with specialists to implement care pathways and coordinate care across the continuum. These care pathways can consider transitions from the acute to post-acute setting, care management handoffs, post-discharge visits and engaging with a post-acute network of high-value providers and facilities to standardize the care path across episodes. Understanding current episodic cost in the post-discharge timeframe and comparisons to benchmarks can provide insight into care plan modifications and where to focus improvement efforts.
The model will also have an element requiring the connection back to primary care services for longitudinal care management – supporting mutual efforts between Accountable Care Organizations (ACOs) and hospitals participating in TEAM.
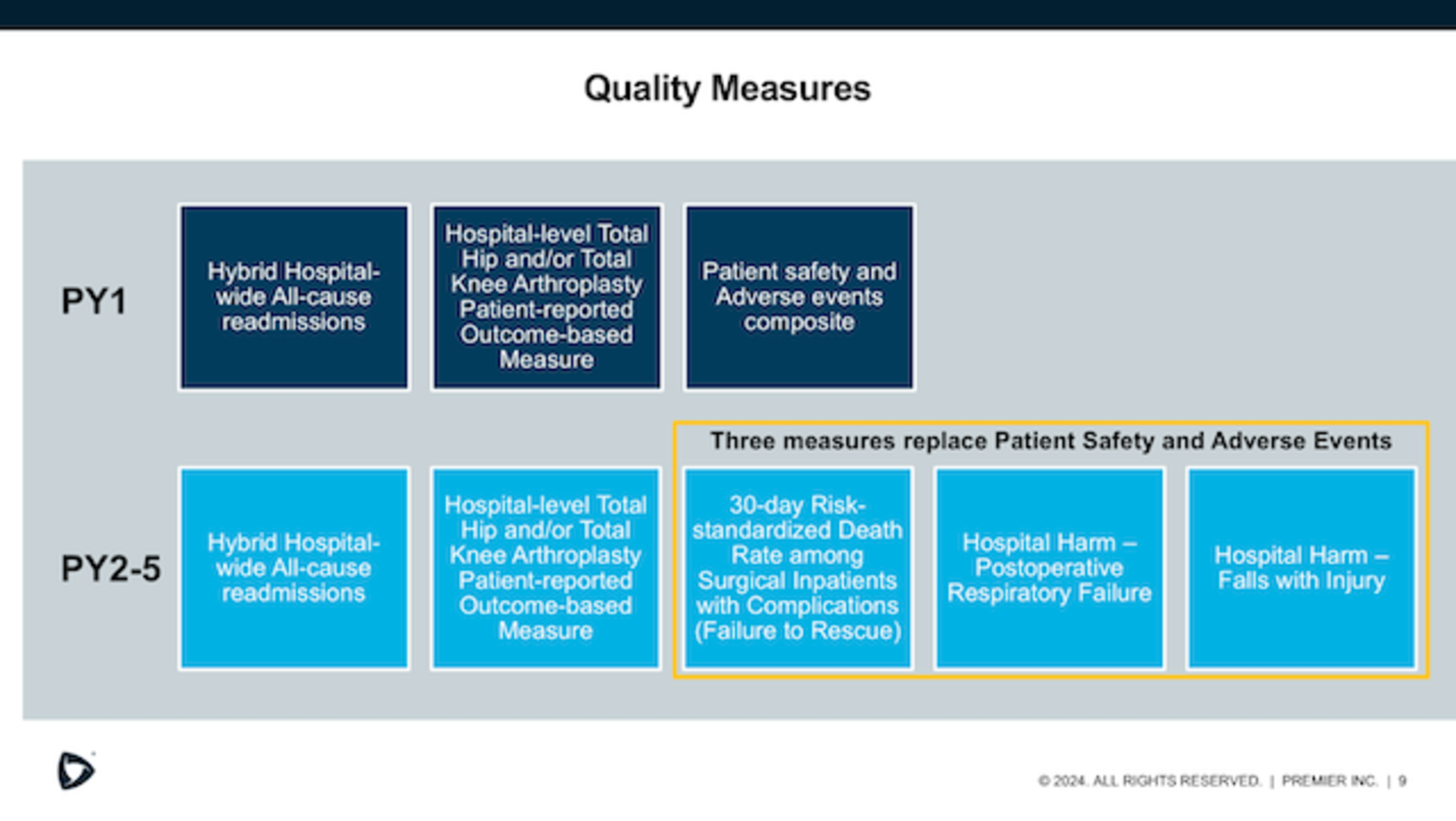
Additionally, while the defined quality measures are already used in ongoing programs (i.e., Hospital Inpatient Quality Reporting (IQR) program and Hospital Acquired Conditions (HAC) Reduction program), they now take on importance as a component for success and earning savings in TEAM. Performance across quality measures will determine the adjustment made to the reconciliation amount – making it more crucial for hospitals to be top performers among the quality measures to receive the full positive reconciliation payment in TEAM.
To succeed in the program, participants must develop effective care pathways and protocols as well as have a strong provider engagement strategy – all of which will demand substantial time and resources. Providers should also consider investing in data analytics and other technologies to monitor patient outcomes and measure performance. Understanding and planning for TEAM participation early in the process is key.
Premier offers a wide range of expertise in TEAM and bundled payment model readiness, preparation, development and implementation.
- Episode Opportunity Analysis: Uses the Medicare 100% Innovator Research Dataset to pull historical claims for all Medicare FFS beneficiaries who would have initiated a TEAM episode if the model was in place. Leveraging the data, Premier provides a dedicated advisor to help pinpoint opportunities for success in the model.
- Organizational Readiness Assessment: Measures core competencies required for successful model implementation. Premier reviews fundamentals with an organization’s team to identify areas in which modifications may be required to achieve improved care and financial success.
- Bundled Payment Collaborative: Connects people, data and knowledge to accelerate improvement in value-based care models. Organizations work together with Premier’s experts and Advocacy team to stay informed on policies, model compliance and model performance. Participating in the Collaborative brings education, shared best practices and advocacy, all of which are important for value-based performance success.
Partnering with over 200 hospitals and physician group practices to support voluntary and mandatory bundled payment programs, we see that engagement with the right partners, utilizing actionable data, leveraging best practices and monitoring ongoing progress help providers accelerate success in bundled payment programs and the transition to value.
Dive deeper and discover how Premier can support your TEAM preparedness and participation.
For More:
- View the on-demand webinar – Preparing for TEAM: CMS' New Mandatory Bundled Payment Model
- See how Premier’s Population Health Management Collaborative (PHMC) members achieved record Medicare Shared Savings Program savings in 2023, outperforming the national average for all ACOs.
- Read the release – Premier Receives 2024 Best in KLAS Award for Value-Based Care Consulting
Wendy Rossi, Vice President
Strategic Collaboratives, Premier
Wendy leads the Bundled Payment Collaborative, which supports participants in episodic value-based models by providing analytics, education and guidance for improvement opportunities.
Kathryn Hayes-Hallowell, Principal
Strategic Collaboratives, Premier
Kathryn is a strategy and operations executive who leads change initiatives aimed at improving quality and costs. Her experience includes: value-based care models (specifically bundled payment), regulatory affairs and performance improvement.
Kathryn is a strategy and operations executive who leads change initiatives aimed at improving quality and costs. Her experience includes: value-based care models (specifically bundled payment), regulatory affairs and performance improvement.
Article Information
Kathryn is a strategy and operations executive who leads change initiatives aimed at improving quality and costs. Her experience includes: value-based care models (specifically bundled payment), regulatory affairs and performance improvement.