Leveraging Data to Improve Quality Outcomes at AdventHealth

Rising healthcare costs, changing health needs and an increased awareness of medical errors are just a few of the factors driving the need for quality improvement in the healthcare industry.
Health systems must combat poor quality health services in order to achieve better healthcare.
Poor quality services offer little value to patients’ health and, in certain cases, may potentially hurt them. Poor quality is also linked to an increase in an organization’s spending because it could lead to unnecessary and costly care.
With government penalties for poor quality and lower reimbursement for care, improving patient quality must remain a top priority for health systems. Healthcare quality can cover effectiveness, safety, a culture of excellence and desired positive outcomes for patients. Defining quality measures and tracking the progress of improvement initiatives is crucial to assess the effectiveness of interventions.
However, often the data available is complex and does not capture the complete picture of quality improvement. The Department of Health and Human Services ensures Medicare payments are tied to meeting minimum standards of quality. Through the Hospital Quality Initiative, the Centers for Medicare and Medicaid Services (CMS) seek to assist hospitals with improving their quality of care. CMS provides public datasets through their Hospital Compare (recently renamed Care Compare) database, utilizing data collected from over 4,000 Medicare-certified hospitals.
There has been a notable rise in consumerism in healthcare, with patients having more choices about where they receive their care. There is greater access to information, leading to the importance of national rankings, such as the CMS Star Ratings.
Healthcare consumers are increasingly using these data sources, which include multiple outcome measures across facilities, to evaluate hospital quality performance before deciding what facility to use for their medical care. Every three years, CMS reviews its standards, which are generally widely accepted among healthcare providers.
Why measuring outcomes is important in healthcare.
AdventHealth has always recognized the importance of reporting outcomes and delivering quality care. “The bottom line is to make sure our patients are well taken care of and that this care is accurately reported,” said Janice Cromer, System Director of Clinical Documentation Integrity.
It is critical for organizations to be effective in impacting the quality of care as well as reporting true quality outcomes that reflect the severity of the patient. AdventHealth has designed, tested and implemented their Quality and Safety of Care Review process (QSR) where they look at all quality outcomes processes, including mortality cases, with a multidisciplinary team. They perform concurrent and immediate post-discharge reviews. The primary focus of the review process is to accurately identify and document reportable conditions capturing the most accurate risk of mortality and severity of illness.

One way to compare outcomes of one hospital to another is through risk adjustment (RA), which AdventHealth relies on as one of their main tools for quality outcomes analysis. One hospital's outcome rate is not comparable to another rate if that hospital takes care of patients at high risk for adverse outcomes.
With RA, there can be an attempt to determine the expected outcome for a group of patients when they are admitted to the hospital based on their known characteristics. A patient with similar characteristics and diagnoses should expect a similar outcome to similar patients.
Risk models let health systems deliver what patients really need.
There are many different risk models out there, but AdventHealth uses Premier's CareScience® analytics as the algorithm. The risk model is driven by Premier's QualityAdvisor™ technology which gains visibility into data insights and benchmark capabilities.
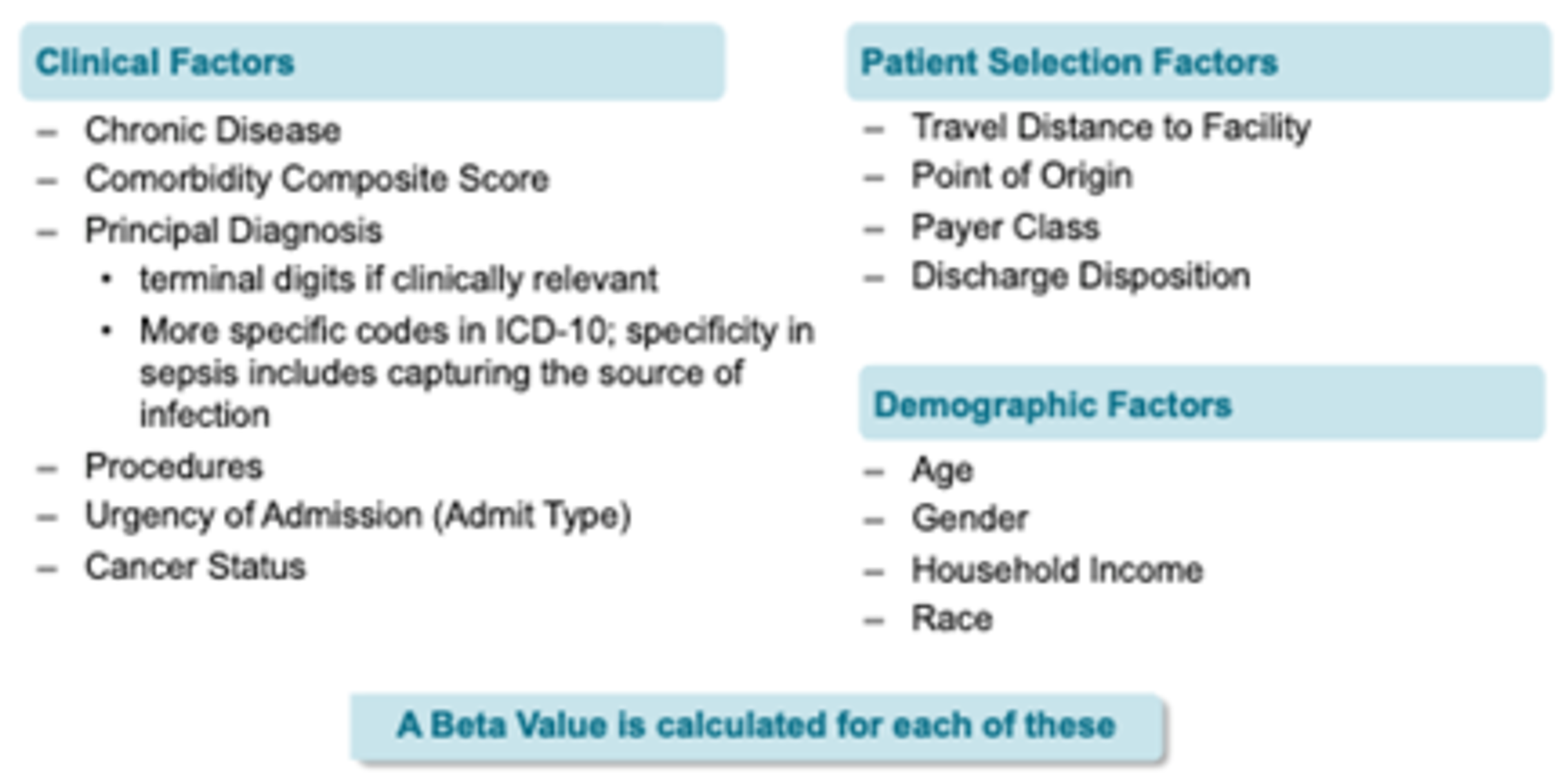
CareScience is very complex and takes into consideration the social determinants of health (SDOH). “We all understand the importance of SDOH, and this is definitely a major focus for AdventHealth,” said Kelly Sutton, RN, System Clinical Documentation Integrity Educator and Implementation Specialist.
That information is used to identify systemic variations in care based on looking at a patient population. The documentation and coding process aims to transform the narrative descriptions to accurately describe co-morbidities, diagnosis and treatment. By doing this, it can impact reimbursement and penalty programs as well as identify false-positive harms.
Premier Healthcare Data contains 20 years’ worth of cost, quality and operational data gleaned from 45 percent of U.S. hospital discharges, as well as 812 million hospital outpatient and clinic encounters and 131 million physician office visits. The database contains a date-stamped log of all billed items and resource utilization during hospitalizations, diagnosis and procedure codes, and patient and hospital characteristics.
Examining the origins of the CareScience methodology.
The CareScience methodology was first developed from a research project at the University of Pennsylvania called the Corporate Hospital Rating Project. The project's goals were to build a new generation of clinical performance improvement tools and isolate patient contributions to outcomes. The project results were a set of multi-variate regression models used to adjust raw inpatient outcomes to control for variations in patient severity. In 2007, Premier acquired CareScience, and the methodology was purchased from the University of Pennsylvania.
The CareScience methodology has been refined each year by Premier data scientists and clinicians during the annual calibration process. The models stay relatively stable from year to year; however, they are stepwise regression models and only retain risk factors that are statistically significantly associated with the outcome of interest for a particular disease. There will be instances when a risk factor may be added or dropped from year to year.
All categories are used for categorical variables in the models; therefore, within the 291 clinical populations across the seven outcomes measures, there could be approximately 300 variables in each model. However, the variable count is lower because a stepwise regression is used to identify statistically significant predictors and remove unnecessary factors.
“Premier gives us a little more in-the-moment view of what our expected mortality is on patients,” said Cromer. “I know we use Premier because it's highly relevant and actionable compared to other sources of data that can sometimes be years old. Rather than using lagging data, CareScience QualityAdvisor data is near real time.”
The CareScience “Risk Calculator" tool was developed and released by Premier in June of 2020 to help organizations educate clinicians and coders on the impact of clinical documentation on the CareScience analytics risk adjustment model.
“The risk calculator tool was a game changer for us as this enabled our team to conduct pre-bill reviews with the risk adjustment model and help manage the observed over expected outcomes,” said Sutton. “This helped all of us to become more aware of what impacts the quality outcomes and made things more actionable. The risk calculator has really enhanced our understanding of the quality outcomes and we were excited when Premier enhanced the risk calculator to auto-upload the patient information into the calculator,” said Tamara Adolph, RN.
Quality improvement made simple.
The goal is to ensure that the accurate severity of a patient at the time of admission is captured in the medical record and subsequently described through available ICD-10 codes and other electronically stored patient data submitted to Premier. “Our job is to assist the physicians in documenting the care they are providing to their patients. Sometimes the physicians think they are documenting the level of specificity needed for outcomes reporting, but oftentimes they are not,” said Adolph.
The coders also benefit from education highlighting the impact of coding with a focus on quality outcomes and overall data integrity. Historically, the industry trend focused on coding for financial reimbursement, creating a dichotomy between coding for Diagnosis Related Group (DRG) reimbursement and coding for quality outcome.
The tool exposes the variables included in the CareScience risk model used to generate an expected risk of an outcome for a patient. Although the tool shows an individual patient's risk, it should be noted that these models are population-based and should not be used at the individual patient level.
Clinicians may be inclined to think of the risk model as taking advantage of all clinical knowledge captured in the electronic medical record (EMR) but can only utilize standardized data extracted from the EMR. To that end, some clinical information may not be included in the risk models that a physician may feel contributed to the patient's outcome.
Utilization of the Premier risk calculator tool in AdventHealth’s QSR process helped to provide educational opportunities not only for the providers and frontline teams, but for their second-level reviewers as well. AdventHealth has initiated an Advanced Practice Forum where their Clinical Documentation Specialists (CDS) who perform the mortality reviews in the QSR process come together monthly to share knowledge with each other. Case studies are presented that highlight how specific diagnoses or the specificity of diagnoses impact the mortality rate based on the use of Premier’s risk calculator. This education can be shared with the frontline teams and providers.
This would ideally be the case; however, the data used for this risk model is taken from thousands of hospitals, so the elements used must be uniformly captured across all hospitals in the U.S. With that in mind, Premier attempts to use as much information as possible through the standardized data to robustly approximate a patient's condition and characteristics in a way that the CareScience methodology provides an estimate of risk at the time of admission.
The CareScience methodology is a statistical model focused on minimizing the variations impacting care and outcomes while capturing the patient’s true clinical status. This is a data-driven statistical approach that incorporates a great deal of clinical and socioeconomical information, and with any statistical model, there will always be outliers and limitations that must be taken into consideration. Overall, data and analytics are becoming increasingly crucial in the transformation of the healthcare system and embracing this notion is the key to improving patient care.