From Bedside to Bottom Line: How Nurse Residency Programs Help Improve Safety, Outcomes and Reduce Labor Costs

Key Takeaways:
- Nurse turnover and vacancy rates across the industry are seeing notable improvements.
- New Premier data shows that hospital-wide agency use has receded – and agency hours and expense for nursing services have decreased.
- Read below and watch the full webinar to see how nursing leaders are supporting workforce retention/recruitment efforts and residency programs.
After nursing workforce losses exceeded 100,000 in 2021, the number of registered nurses (RN) employed in the profession has slowly begun to recover. Healthcare providers are making significant investments in workforce retention efforts – and nationally, there is a shift towards less reliance on premium pay.
Recent reports show that nurse turnover is returning to near pre-pandemic levels at 18 percent, and 40 percent of hospitals are reporting RN vacancy rates below 7.5 percent.
Premier data mirrors these trends. A new Premier analysis reveals that hospital-wide agency use has receded – from a median high of 3.8 percent in 2022 to 1.4 percent for the 12 months ending Sept. 30, 2024.
For nursing services, median agency hours dropped from 3.5 percent to 2 percent, and median agency expense (as a percent of total labor spend) dropped from 8.4 percent to 3.4 percent over the same time period (Table 1). And while RN agency utilization has decreased since its peak, it remains slightly higher through Q3 2024 compared to pre-pandemic levels.
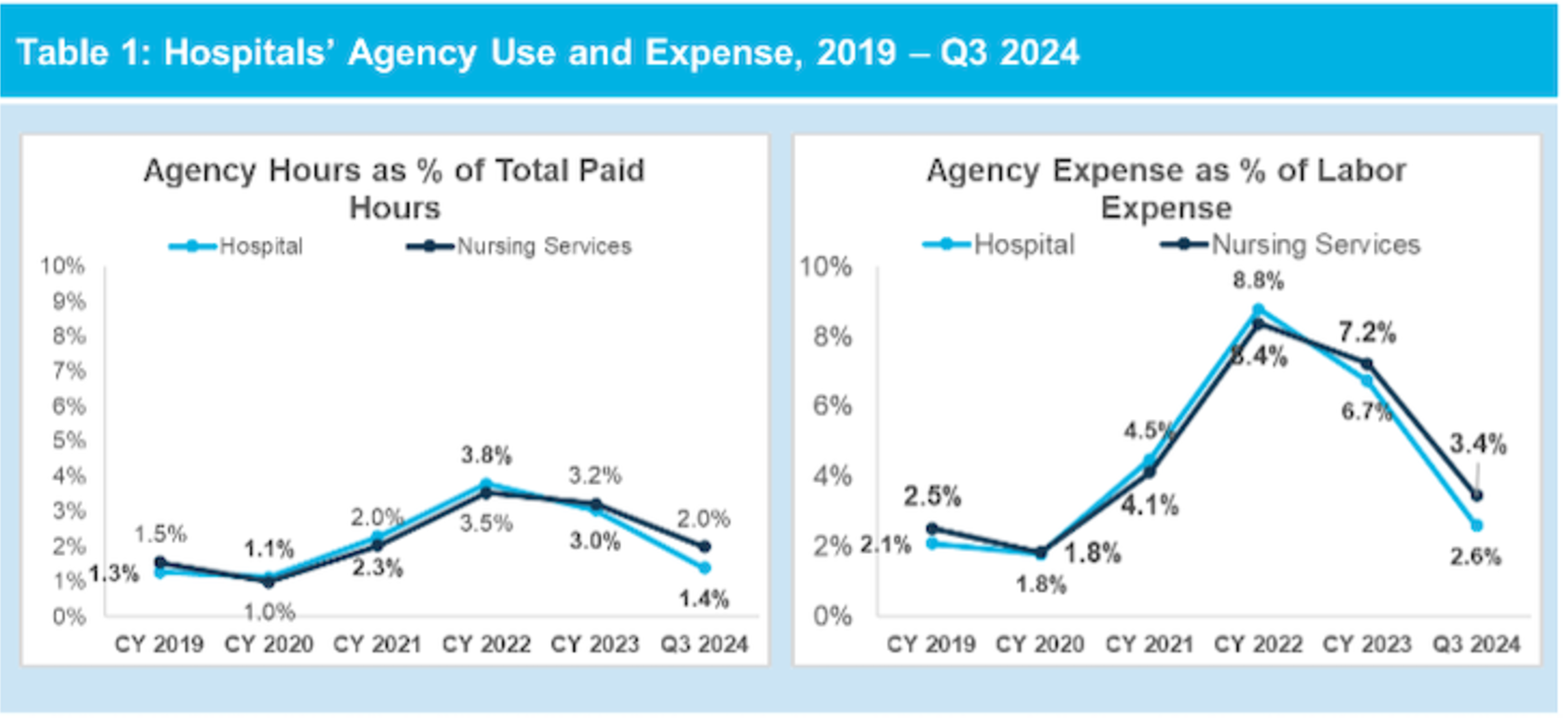
Source: Premier OperationsAdvisor® benchmarking data.
Premier’s analysis leverages robust workforce benchmarking data from over 650 healthcare organizations to help optimize productivity and identify improvement opportunities.
Nursing Leaders Share Key Strategies for Workforce Optimization Efforts and Residency Programs
Healthcare leaders are deploying a broad range of strategies to support nurse retention, including:
- Competitive compensation and benefits.
- Career development and growth opportunities.
- Renewed focus on a healthy workplace culture.
- Enhancements in communication, feedback and recognition systems.
- Flexibility in scheduling and staffing models.
- Innovations in onboarding models.
Many nursing leaders are also finding significant return on investment in nurse residency models for new nurses – also often referred to as transition to practice (TTP) programs.
Generally, TTP programs help new nurses or those re-entering the workforce develop the skills and confidence to provide safe, effective patient care. Most TTP models include core proven practices, including:
- Structured program with measurable outcomes
- Preceptor training and support
- Progressive increase in responsibilities
- Emotional and psychological support
- Cultural integration
- Data-driven insights to transition progress and success
- Evidence-based practice/quality improvement projects
- Use of high-fidelity simulation safe learning
Yet even with the scale, operations and resources to develop and implement TTP programs, many acute care organizations still face barriers to success such as access to professional development resources (human and technical), managing operations across geographies, and developing peer-to-peer networks both internally and externally with other health systems.
Premier’s Workforce Innovation Collaborative recently gathered nursing leaders for a webinar to discuss the value of tech-enabled TTP models – and how these programs can support employee satisfaction and a hospital’s bottom line. Four key themes emerged during the panel, moderated by Dawna Cato, PhD., RN, NPD-BC, Director, Residency Programs at OpusVi:
Nursing retention as a business strategy.
The role of strong preceptors and preceptor training.
Technology to assess residents’ progress and TTP program efficacy.
Technology to shore up program gaps and expand professional networks.
Nursing Retention as a Business Strategy
Recent studies show the average cost of turnover for a staff RN was over $56,000 in 2024 – and each percentage point change in RN turnover equates to about $263,000 in cost or savings for the average hospital.
“Our nurse residency program has been implemented in 75 percent of our hospitals and our aggregate retention is 91%.” – Jennifer Hubek, MS, RN, NPD-BC, System Director, National Nurse Residency Program, CommonSpirit Health on the impact of deploying a robust, evidence-supported TTP program at the organization.
“Our TTP program not only helped us with nurse retention, but also with recruitment. In the past, we lost several nurse prospects when we did not have a TTP program. Since implementing the program, we were able to fill almost every vacancy every semester for the last three semesters” – Kristin Grimes, MSN, RN, CIC, Assistant Manager, Med/ Surg and ICU, Mount Graham Regional Medical Center
In addition to operational costs, nursing leaders attending the webinar shared that patient outcomes and employee satisfaction scores were key measures monitored for improvement (Table 3). Grimes echoed attendees’ responses: “We tripled our overtime cost savings, reduced our use of agency nurses… and saw our patient satisfaction scores improve… specifically with discharge planning.”
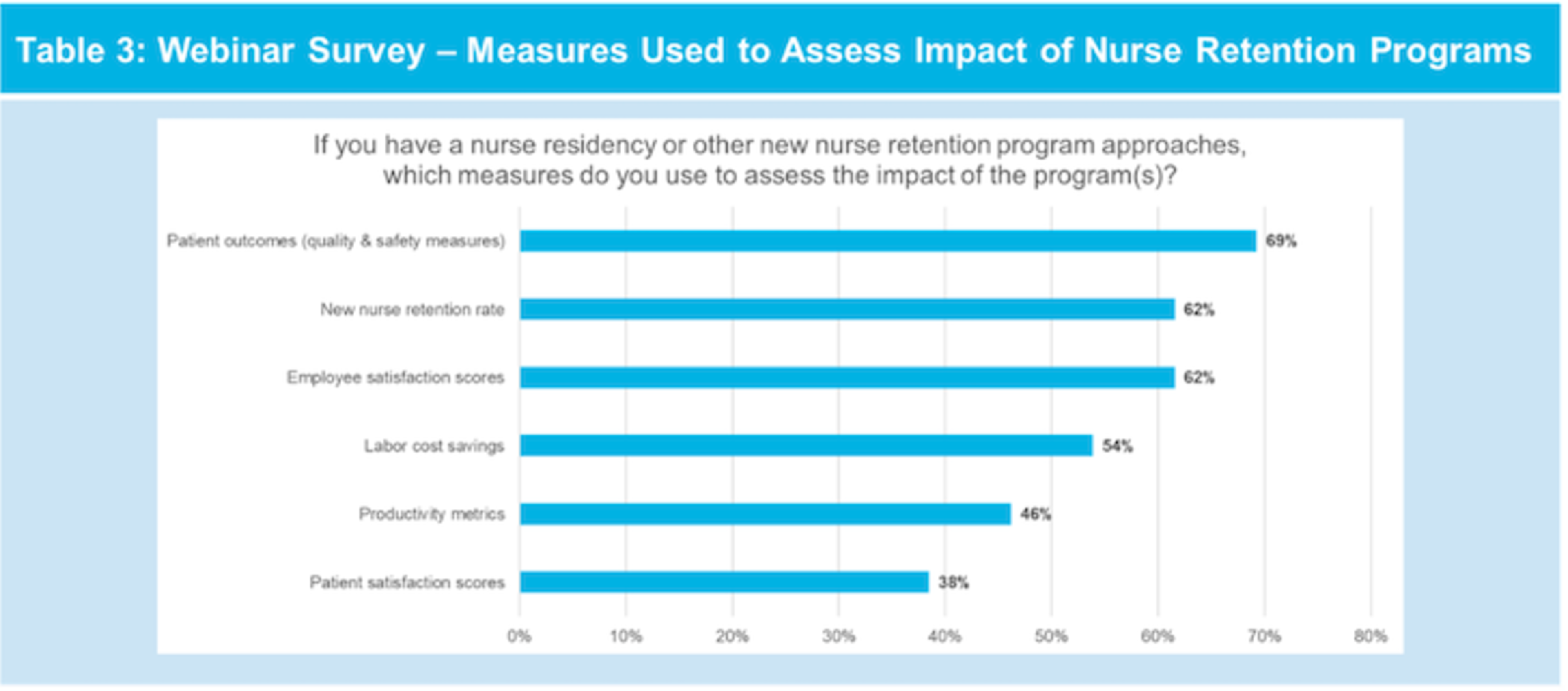
Source: Premier survey conducted on Jan. 23, 2025.
The Role of Strong Preceptors and Preceptor Training
World-class preceptors and preceptor training programs can have a positive effect on RN retention rates, confidence and job satisfaction for new-to-practices nurses.
Our preceptor model is huge for our preceptors and residents… it really helps build our new graduates’ confidence to go through clinical skills with someone that has experience beside them.” – Dr. Marsha Yembi, EdD., MSN, RN, Market Director, National Nurse Residency Program, CommonSpirit Health
Hubek added detail on the CommonSpirit Health model: “The role of preceptors and their training is critical… we also assign the residents mentors after orientation… we have a well-being curriculum with topics such as resilience and decompression, CommonSpirit values, opportunities to discuss what’s happening on their units and a career coach to meet individually with residents to support their own growth.”
“One benefit of the preceptor program has been that our new nurses now feel like they have a “go-to” person to ask those questions that they might feel like are silly or insignificant… but they’re important to patient care,” shared Grimes.
Technology to Assess Residents’ Progress and TTP Program Efficacy
Harnessing data for actionable insights is critical to understanding how new-to-practice nurses are progressing and for pinpointing ways to support their success. Yet TTP programs are often decentralized, thus requiring tight coordination between program administrators and front-line preceptors.
To address this, healthcare providers are adopting technology solutions to help track a nurse resident’s knowledge retention, willingness to actively engage in the program and completion of learning objectives. Data collected throughout the resident’s journey enables highly personalized intervention and optimization.
According to Hubek: “We have a technology-enabled process to review our preceptors’ evaluations of nurse residents and their progress each week… we discover things early so we can intervene early.”
Technology to Shore Up Program Gaps and Expand Professional Networks
In some instances, internal nurse residency models may lack elements to ensure they are efficient and effective – hampering an organization’s ability to achieve desired results. Among the nursing leader webinar attendees, 29 percent reported that their organization’s program is internally developed and not credentialed through an external partner, such as ANCC Practice Transition Accreditation Program® or AACN Commission on Collegiate Nursing Education (Table 4).
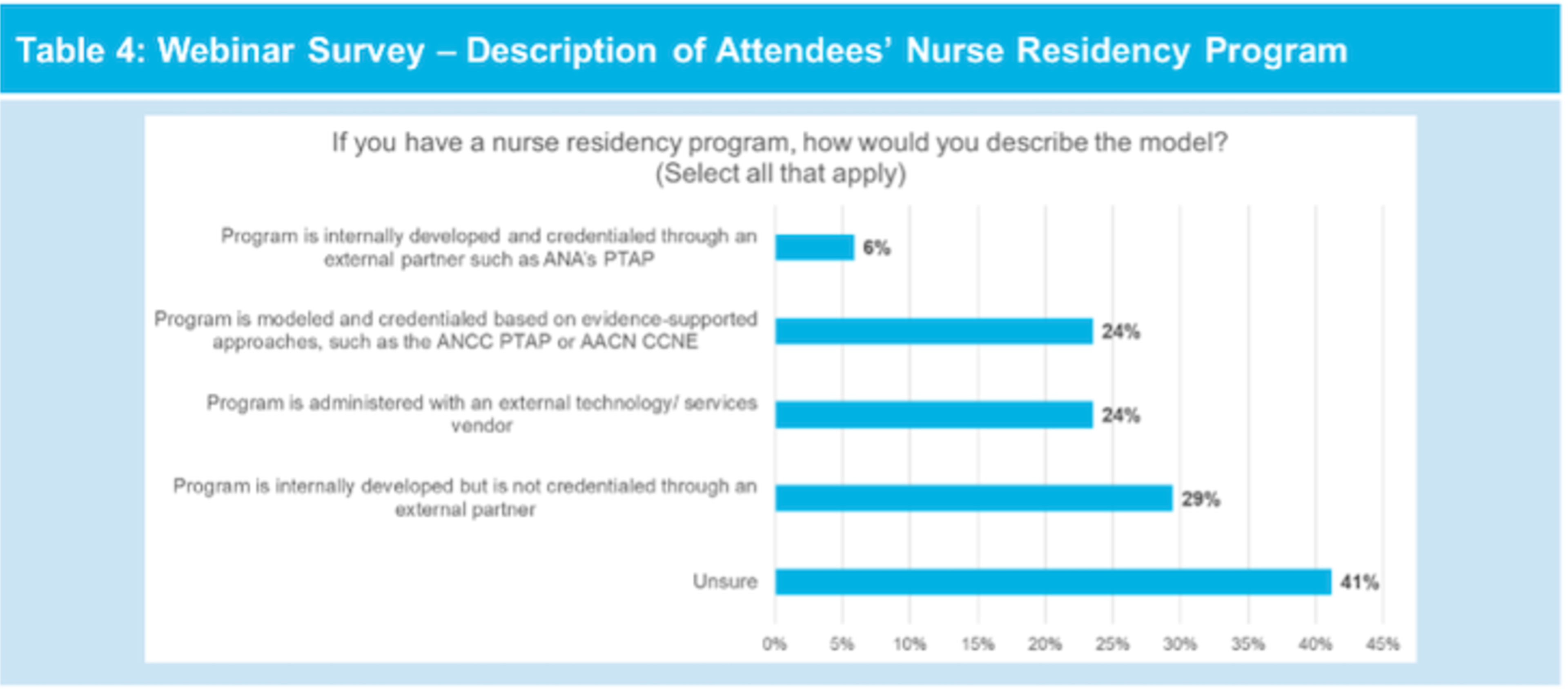
Source: Premier survey conducted on Jan. 23, 2025.
Grimes described organizational challenges and how a tech-enabled approach has helped: “Being a rural critical access hospital, we have unique challenges. We did a gap analysis and quickly realized we had opportunities to improve our curriculum guidelines for new graduates. We used a technology platform to strategically align our education resources for each area.” Perhaps most importantly, she added, “When you’re developing your program… you should include your front-line staff and talk about what their needs are. Then promote that with program leadership.”
Solutions for healthcare’s workforce challenges are as broad as the underpinning factors that drive modern-day issues. Nurse residency programs, as well as data and technology to scale these programs, are just one of the ways to grow and sustain one of healthcare’s most valuable assets.
Cato shared: “We can no longer wait for nurses to gain professional growth by having them spend two-to-five years on med/surg units… we need innovative strategies to get them ready to progress more quickly.”
Nurses’ appetite for professional growth is moving at the speed of change – is your organization ready?
Contact Thomas Flynn, Principal, Strategic Collaboratives, to learn how Premier’s Workforce Innovation Collaborative connects health systems with actionable data and shared best practices to help solve unique workforce challenges.
Premier will continue to offer live, curated workforce thought leadership through our webinar series and Workforce Innovation Collaborative National Meeting in Washington, D.C., on July 15, 2025.
Learn More:
- See how Premier's advisory services team can help your organization unlock efficiency and improve outcomes with a Healthcare Rapid Assessment.
- Discover how Beebe Healthcare optimized its workforce and implemented sustainable operational changes with Premier as its partner.
- Take a deeper dive into Premier’s technology and advisory services that support workforce and performance improvement efforts.
I’m a healthcare improvement professional who designs, implements and provides leadership oversight for solutions that improve the quality, efficiency and cost of healthcare. I have a diverse blend of clinical, operational and analytical experience that spans pre-hospital, acute, chronic and long term care. When I’m not working, you’ll find me riding/racing bicycles through the woods or spending time with my son camping, snowboarding or nagging him to do chores.
Article Information
I’m a healthcare improvement professional who designs, implements and provides leadership oversight for solutions that improve the quality, efficiency and cost of healthcare. I have a diverse blend of clinical, operational and analytical experience that spans pre-hospital, acute, chronic and long term care. When I’m not working, you’ll find me riding/racing bicycles through the woods or spending time with my son camping, snowboarding or nagging him to do chores.