Lack of Standardized Data Collection Impedes Efforts to Advance Health Equity

Key takeaways:
- The process of social determinants of health (SDOH) data collection and analysis should be standardized across hospitals and health systems to advance health equity.
- Data integrity across all health systems is a key component for success when working with equity-related data, metrics and resources that illuminate disparities in care.
- A standardized SDOH data collection method and its results can influence policy aimed at advancing equity and reducing disparities.
Understanding Health Equity
Health equity is a broad term that the Centers for Disease Control and Prevention (CDC) defines as each person having the chance to reach “his or her full health potential” without facing obstacles from “social position or other socially determined circumstances.”
Influences on health equity include SDOH which, according to the Department of Health and Human Services (HHS), are “the conditions in the environments where people are born, live, learn, work, play, worship and age” that affect a wide range of health, functioning and quality-of-life outcomes and risks. Examples include community-level issues such as educational access and aspects of the neighborhood in which one lives. On an individual level, health-related social needs (HRSN) are individual, person-specific challenges, including food insecurity and personal safety, that have an immediate and direct effect on health outcomes.
Influences on Health Equity: Three Areas of Social Circumstances
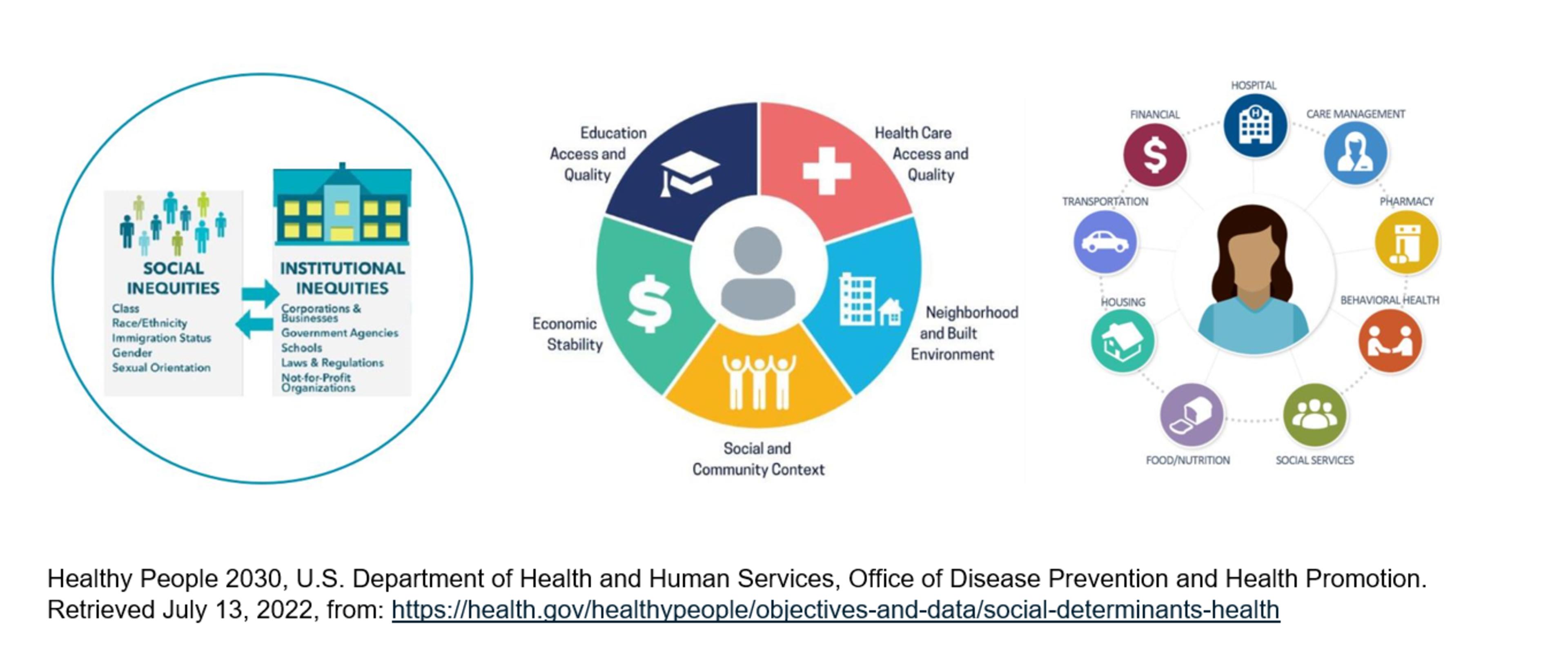
Many people in the U.S. do not get the healthcare services they need. It can be for a variety of reasons but there are three social circumstances that are known to impact an individual’s health.
- Structural - systemic and institutional mechanisms, including policy that organizes the distribution of power and resources differentially across lines of race, gender, class and sexual orientation.
- Community – issues or SDOH in the environment where people are born, live, work, play and exist and how these factors impact health and/or quality of life.
- Individual – HRSNs are more immediate real-time gaps that obstruct a person’s health, wellbeing and safety. Short term gaps in the ability to achieve optimal health don't come from the traditional healthcare system, such as access to transportation, food and behavioral health services.
Health Equity: A National Priority
The COVID-19 pandemic raised public awareness of health disparities which has resulted in health equity becoming a national priority.1
The Biden-Harris Administration’s blueprint to improve the health and wellbeing of individuals and their infants in America includes the launch of the Maternal Morbidity and Mortality Data and Analysis Initiative with Premier, as well as a maternity care quality hospital designation and SDOH data collection requirements in the FY23 IPPS Rule.2,3,4,5
Building upon the Administration’s commitment to advance racial equity and support for underserved communities, the Centers for Medicare and Medicaid Services (CMS) developed a strategic plan consisting of six pillars.6,7 Their initial pillar of focus is concentrated on addressing these disparities and advancing health equity.8 CMS has started to include health equity-related elements in many of its programs, and other payer and policy organizations are following suit.
Although efforts like these are just getting started, they are key to helping improve the nation’s overall health and economic prosperity. One analysis estimates that disparities amount to approximately $93 billion in excess medical care costs and $42 billion in lost productivity per year, as well as additional economic and human losses due to premature deaths.
Reducing Inequities: Understanding Patient Needs and Using Customized Tools
As maternal mortality and morbidity continue to rise, the need to understand and address differences in outcomes based on race and ethnicity has never been greater. For example, according to the CDC, Black individuals are three times more likely to die as a result of pregnancy or childbirth, and social factors play a large role in their outcomes. They also have a higher rate of eclampsia, preeclampsia, diabetes, cardiovascular disease and obesity. Lastly, we know that medical conditions impact economic conditions which in turn impact overall health.
“Our healthcare has gotten better, yet women are still dying because they are bleeding to death postpartum. Why haven’t we been able to solve for postpartum hemorrhage? We must work to understand the “why,” said Dr. Betty Chu, Associate Chief Clinical Officer at Henry Ford Health System.
Improving disparities goes so much further than addressing a patient’s visit to their physician where they receive treatment, prescriptions for medications and advice regarding diet.
If an individual takes time off from work to handle clinical appointments, that has a financial impact. If he or she has difficulty accessing transportation to clinical appointments, this adds another layer of complexity. And if a patient doesn’t have access to a grocery store that offers healthy foods, health disparities can ensue.
Keeping up with these socioeconomic elements that impact care is daunting. Clinicians care about their patients and want them to obtain optimal care, but it is hard to gather all the factors impacting a patient during a routine office visit. Not to mention, this is sensitive information that can be challenging for patients to share and for clinicians to keep updated.
It’s clear that a solid infrastructure is needed to collect and store data in electronic medical records (EMRs) in a standardized way. How we collect these elements is the bigger question. Do clinicians hire a dedicated staff member to collect SDOH during check-in or utilize technology such as a tablet, where patients input their information discreetly?
Patients need to feel comfortable when sharing this sensitive personal information, and they are more likely to do so when they have an established patient-clinician relationship built on trust and respect.
Maintaining that trust and openness to share requires utilizing customized tools that fit populations’ needs, and each tool requires thought and resources for execution and data connectedness with community resources and referrals that can provide interventions to improve outcomes.
Lack of Standardization Impacts Improvement
Despite the importance of reducing health disparities, the U.S. is challenged by the fact that there isn’t a standardized method of collecting or analyzing SDOH or HRSN data. Measuring improvement in outcomes that are impacted by these socioeconomic factors requires standardized data that can provide insights into what needs exist, which evidence-based interventions could help and how a healthcare facility compares over time and against its peers using national benchmarks.
“We knew there would be a lot of variability in the collection, storage and analysis of these data. In order to streamline operational effort, we wanted to explore which data elements should be prioritized for collection in a standardized way so that they can be examined for casual associations to improve health outcomes,” said Dr. Tracy Hoke, Chief Quality and Performance Improvement Officer at University of Virginia Health.
Premier and nine academic medical center members came together to understand how hospital and health systems in the U.S. could benefit from a standardized collection method. With access to more than 400,000 patient records, they began by conducting a research study to address SDOH and HRSN data collection, storage, transmission and aggregation so there could be shared understanding of how that data could be used effectively to reduce health disparities.
Sadly, researchers found there wasn’t a standardized method for collecting SDOH elements at any of the academic medical centers that shared data.
“Currently, it’s hard to rely on SDOH data to inform evidence-based best practices, make quality improvements or inform policy decisions when there is so much variability in the data set. We know that health systems aren’t collecting the same data elements in the same way, and we need to standardize processes to understand the impact of risk so that deliberate interventions can be designed to advance outcomes,” said Dr. Tracy Hoke.
Ensuring Data Integrity
Moving forward, data integrity will play a key role in efforts to advance health equity and reduce disparities. Without a standardized process in place, there will be little chance of measuring improvements or scaling best practices.
“We all have EMR data that contains great variation in measuring and reporting SDOH,” said Dr. Peter Pronovost, Chief Clinical Transformation Officer and Chief Quality Officer, University Hospitals Health System. “But if we don’t get this right, we’ll never know if we’re making an impact on reducing the three-fold higher rate in Black maternal deaths.”
Everyone will need to work together to ensure collection of the right SDOH data that impacts patients, their health outcomes and chances of mortality to bolster these socioeconomic gaps through policy changes, access to community and patient support.
Efforts must be aimed at reducing harm, driving clinical quality improvements, advancing health equity and reducing disparities for all.
Advancing Health Equity Through Collaboration
Premier continues to focus efforts on advancing health equity by bringing together clinicians, health systems and life sciences companies to address the drivers of disparities and inequities and how to reduce them across all areas of healthcare, together.
Reducing disparities across health outcomes will require a diverse and inclusive healthcare environment where all patients can thrive and receive optimal health outcomes.
Premier’s Health Equity Collaborative participants will work together to:
- Engage in shared learning for best practices on assessment of patients’ social needs and the development of a health equity action plan, while also minimizing burden to existing staff.
- Improve health equity and reduce disparities by standardizing SDOH data collection.
- Innovate the future of health equity improvement with patient-specific social needs data, a unique health disparities index to support benchmarking and help guide policy development.
Find out how you can join Premier’s Health Equity Collaborative, learn more about this ongoing study or get involved in the design and implementation of methods to improve equity by completing this form.
Further Reading:
- Access CMS’ Final Inpatient Prospective Payment System FY 2023 (IPPS) Rule.
- Learn more about Premier's Applied Science’s Maternal Health Database and learn how its data can inform your maternal and infant health improvement efforts.
Sources Cited:
- FACT SHEET: Vice President Kamala Harris Announces Call to Action to Reduce Maternal Mortality and Morbidity. (2021, December 7). Retrieved August 15, 2022, from https://www.whitehouse.gov/bri...
- White House Blueprint for Addressing the Maternal Health Crisis. (2022, June). https://www.whitehouse.gov/wp-...
- Maternal Morbidity and Mortality Data and Analysis Initiative. (2021, December 14). The U.S. Department of Health and Human Services Office on Women’s Health. Retrieved August 15, 2022, from https://www.womenshealth.gov/a...
- FY 2023 Hospital Inpatient Prospective Payment System (IPPS) and Long Term Care Hospitals (LTCH PPS) Proposed Rule - CMS-1771-P (Maternal Health). (2022, April 18). The Centers for Medicare and Medicaid Services. Retrieved August 15, 2022, from https://www.cms.gov/newsroom/f...
- FY 2023 IPPS Final Rule Home Page. (2022, August 1). The Centers for Medicare and Medicaid Services. Retrieved August 15, 2022, from https://www.cms.gov/medicare/a...
- Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government. (2021, January 20). The White House. Retrieved August 15, 2022, from https://www.whitehouse.gov/bri...
- CMS Strategic Plan. (2022, August 3). The Centers for Medicare and Medicaid Services. Retrieved August 15, 2022, from https://www.cms.gov/cms-strate...
- CMS Strategic Plan Pillar: Health Equity. (2022, August). The Centers for Medicare and Medicaid Services. https://www.cms.gov/files/docu...
The insights you need to stay ahead in healthcare: Subscribe to Premier’s Power Rankings newsletter and get our experts’ original content delivered to your inbox once a month.

Carolyn is a nurse executive with a 25-year record of leadership in established and start-up healthcare organizations. At Premier, she oversees strategy and leads award-winning teams focused on value-based care delivery, population health, maternal and infant care, and academic affinity groups, as well as newer initiatives focused on transformation of the healthcare workforce, health equity and redesign of oncology services.

Dr. Madeleine Biondolillo is vice president, quality and safety at Premier, where she is responsible for growth of strategic quality and population health initiatives to support members in value-based healthcare delivery improvement. When she's not working, her hobbies are running half-marathons and volunteering in organizations that support victims of domestic violence.
Article Information

Carolyn is a nurse executive with a 25-year record of leadership in established and start-up healthcare organizations. At Premier, she oversees strategy and leads award-winning teams focused on value-based care delivery, population health, maternal and infant care, and academic affinity groups, as well as newer initiatives focused on transformation of the healthcare workforce, health equity and redesign of oncology services.

Dr. Madeleine Biondolillo is vice president, quality and safety at Premier, where she is responsible for growth of strategic quality and population health initiatives to support members in value-based healthcare delivery improvement. When she's not working, her hobbies are running half-marathons and volunteering in organizations that support victims of domestic violence.