Premier Data: Navigating Patient Access Challenges to Enhance Care and Grow Revenue

Key Takeaways:
- New Premier data shows, on average, a 53 percent increase in lead times across all specialties with larger spikes in some areas since 2020.
- Virtual visits have dropped nearly 50 percent since 2020 across all specialties.
- Leveraging innovative data and technology platforms to address strategic and operational challenges, providers can make care more accessible and grow revenue.
Patient access is a key driver of patient acquisition, satisfaction and retention – all of which deeply influence care quality and provider revenue. Today, patients seeking convenient and timely care options gravitate toward providers who offer optimal access, whether that means shorter wait times, flexible scheduling or easy connections to specialty services.
Access to care – once a consideration in deference to quality of care – is now a primary factor affecting where patients choose to receive services. Indeed, patient access plays a direct, critical role in providers’ ability to achieve strong outcomes.
New Premier Data Points to Contributors of Patient Access Challenges
Lead times for new patients – the average number of days between a patient’s initial appointment request and completion of the appointment – continue to rise. Premier data shows, on average, a 53 percent increase in lead times since 2020 across all specialties with larger spikes in some areas:
- +74 percent for primary care advanced practice providers (APPs)
- +67 percent for primary care physicians
- +57 percent for medical specialist APPs
- +67 percent for hospital-based physicians

Source: Premier Physician Practice Benchmarking (PPB) data; N=60,000+ providers
The rise of retail health clinics and telehealth services, both of which offer convenient alternatives to traditional care models, helped kickstart the current focus on access.
Yet, virtual visits – a key component of successful patient access strategies – have declined significantly since the height of the COVID-19 pandemic. Premier data shows that virtual visits have dropped nearly 50 percent across all specialties since 2020.
Even providers that use virtual visits the most (defined as 20 percent or more of all visits delivered as a virtual visit) saw drastic drops since 2020, including:
- -30 percent for allied health
- -45 percent for medical specialist APPs
- -57 percent for medical specialist physicians
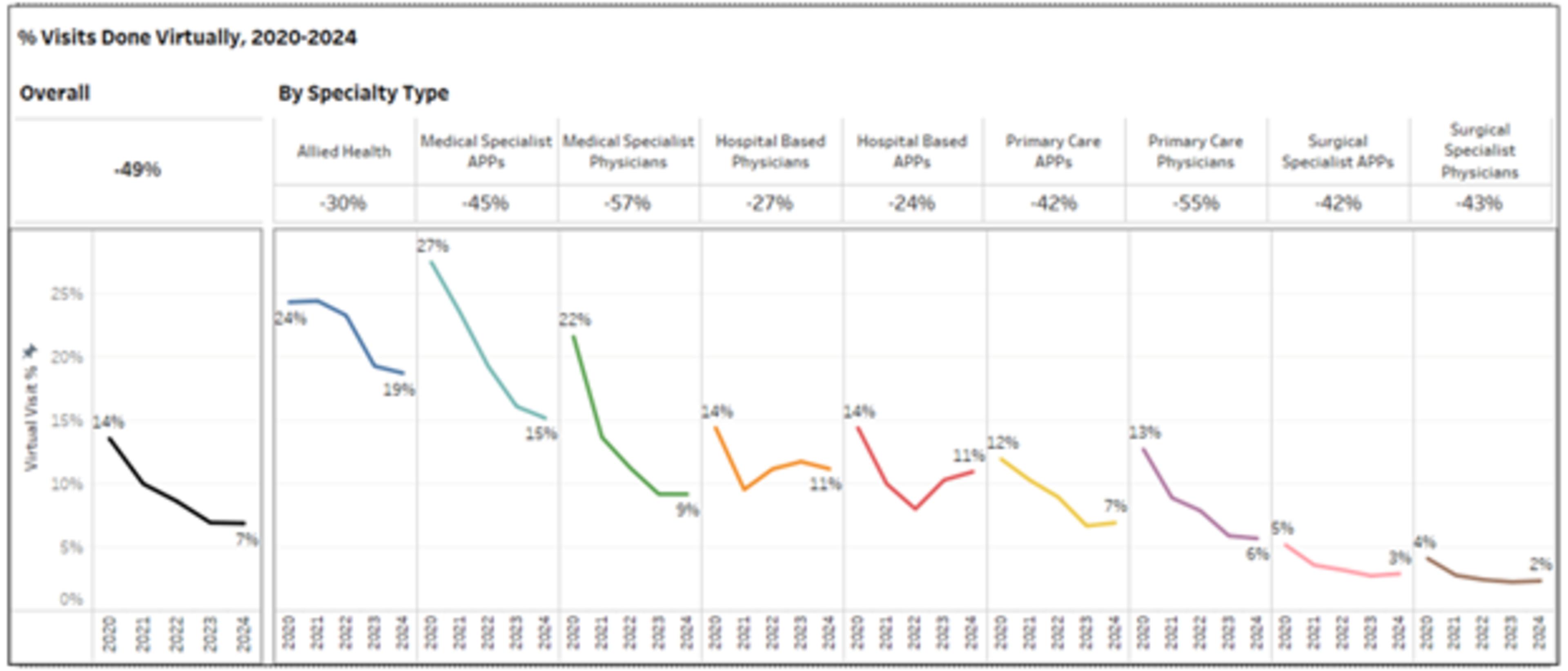
Source: Premier Physician Practice Benchmarking (PPB) data; N=60,000+ providers
Telehealth is a largely untapped opportunity, but realizing its full potential requires a thoughtful approach. For example, should it be synchronous or asynchronous? Are the right workflows in place to ensure a streamlined experience and appropriate care delivery? More education is also needed to ensure patients understand when and how to schedule a virtual visit instead of a traditional appointment.
Market Forces Contribute to Strategic and Operational Challenges that Strain Access to Care
Providers are not immune to the burdens of inflation – namely higher material and labor costs – putting leadership under intense pressure to protect operating margins. Physician groups and hospitals are also charged with retaining both clinical and non-clinical staff to keep up with growing patient access demands.
At the same time, patients are becoming more empowered and informed consumers. They are demanding more transparency, convenience and quality from their healthcare providers. This, in turn, is intensifying competition among providers to win the business of patients who are shopping around for the best patient experience and greatest value.
To address patient access problems, organizations must first identify the root causes. Do their providers have capacity? Are they in the right locations? Do they offer appointments at the right times? And, if capacity exists, are open windows being offered to patients? Can patients easily schedule in-person and/or telehealth appointments?
LeveragingData, Technology and Advisory Expertise for More Accessible Care
Healthcare providers must adapt to meet heightened expectations regarding access. Patients are now accustomed to on-demand services in nearly every sector. If they encounter long wait times, limited appointment options or a cumbersome scheduling process, they are likely to seek care elsewhere.
Using advanced data and innovative technology platforms, Premier Advisory Services helps providers across the care continuum co-design, implement and optimize a cohesive patient access and retention strategy.
Healthcare organizations can start by committing to a renewed, strategic focus on access metrics. However, benchmarking against generic peer groups or industry cohorts will not fuel success. Rather, providers must assess performance against direct competitors in the market. This localized benchmarking mirrors how patients make decisions – thus empowering health systems to become the provider of choice in their communities.
Premier’s Provider Practice Benchmarking solution, which collects and processes data from over 60,000 physicians and APPs working in over 8,000 practices nationwide, helps provide medical groups with the insights they need. By analyzing billing, scheduling, payroll and financial data, Premier’s platform helps organizations identify gaps, inefficiencies and opportunities in real time.
Solutions that promote more personalized care are also imperative. Premier’s Quality Improvement technology includes analytics and clinical benchmarking as well as clinician performance management – all designed to help providers maximize efficiencies and quality outcomes. And Premier’s Stanson Health provides tailored, evidence-based recommendations at the point of care for timely and pertinent treatment decisions.
For providers, advisory experts can help maximize the appropriate technology, tools and actionable data to meet operational, patient access and quality care goals. Premier’s Advisory team helps a provider’s team pinpoint unique needs and leverage technology for greatest value – regardless of where an organization may be in its digitization journey.
Premier’s Government Affairs team acts as an advocate for Premier members and the communities they serve. Premier successfully advocated for an expansion of telehealth during the pandemic and is now supporting permanent policy changes to modernize the Medicare telehealth benefit. These efforts are aimed at helping ensure that more patients have access to telehealth services and that providers are adequately reimbursed for them.
Putting It All Together
A successful access strategy calls for a coordinated care model that focuses on patients’ needs and experiences. Providers must move from disconnected to integrated; measure and monitor defined access metrics in real-time; and make smart investments in people, processes and technology that support organizational growth while keeping the patient experience front and center. Above all, solutions must be sustainable to provide both immediate and long-term value to patients and providers.
Creating a robust access operating model is a journey, not a sprint, and it requires a strategic approach. The rewards, however, are substantial: Advancing patient access is not only the right thing to do, but also one of the most effective ways to improve revenue at a time when providers are facing increased costs across the board.
Learn More:
- Explore key healthcare data and technology challenges and discover specific steps you can take to achieve resiliency, standardization and consistency.
- Discover how Premier’s advisory services team helped East Carolina University (ECU) Health Physicians create $10.7 million in revenue enhancement.
- See how Premier's advisory experts can help your organization unlock efficiency and improve outcomes with a Healthcare Rapid Assessment. We work with healthcare organizations to quickly pinpoint areas of improvement and deliver actionable insights for meaningful change.
Dr. DeBehnke is a member of Premier's Advisory Services team where he leads consulting engagements in the areas of large-scale clinical transformation, clinical variation reduction and ambulatory operations improvement.
Article Information
Dr. DeBehnke is a member of Premier's Advisory Services team where he leads consulting engagements in the areas of large-scale clinical transformation, clinical variation reduction and ambulatory operations improvement.