Claims Adjudication Costs Providers $25.7 Billion - $18 Billion is Potentially Unnecessary Expense

Key Takeaways:
- Claims adjudication cost healthcare providers more than $25.7 billion in 2023 – a 23 percent increase from the previous year.
- 70 percent of denials were ultimately overturned and the claims paid, but only after multiple, costly rounds of review.
- Premier’s solutions help bridge the gap between payers and providers – optimizing resource utilization, streamlining administrative processes, ensuring accurate reimbursement and improving outcomes.
Claims adjudication costs healthcare providers more than $25.7 billion, according to a new national survey of hospitals, health systems and post-acute care providers conducted by Premier, Inc. This figure represents a 23 percent increase over the $19.7 billion in costs reported in the previous year.
Claims move into the adjudication process after payers issue an initial denial on the submission. While denial rates remained consistent at nearly 15 percent, according to survey data, they ranged as high as 49 percent in certain instances.
In addition, the administrative costs associated with fighting them increased dramatically – from $43.84 per claim in 2022 to $57.23 in 2023. Additional costs primarily resulted from added labor, responsible for 90 percent of claims processing expenses incurred by providers.

Health insurers process about three billion medical claims annually, and approximately 70 percent of denials are overturned and paid. This means that nearly $18 billion was potentially wasted arguing over claims that should have been paid at the time of submission (see Methodology section for more detail).
This continued burden has a tremendous impact on providers’ financial viability. Over the past year, the average number of days of cash on hand for hospitals and health systems overall dropped to 196.8 days, the lowest level in a decade. When providers lack cash on hand, they are unable to re-invest in patient care and may also suffer from downgrades in bond ratings, making cash more expensive and harder to obtain.
In addition, the cost of adjudicating claims reported by Premier’s research does not include those incurred by payers, which average $40 to $50 per submission. Similar to providers, these costs contributed to a 7 percent (or $4 billion) increase in net administrative costs in 2023 across the insurance sector. The added administrative costs match premium increases in 2023, which also grew by 7 percent. Cutting these administrative costs from the healthcare landscape could potentially reduce premium increases faced by consumers.
Prior Authorization: A Broken Reimbursement Process
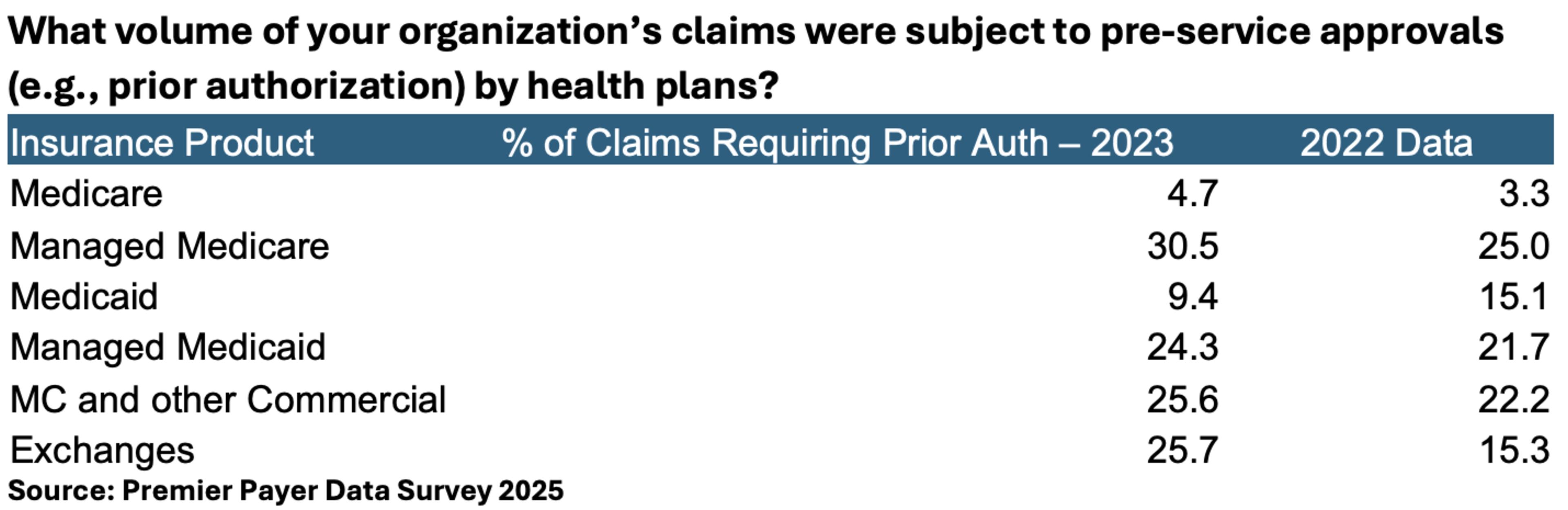
Payers required prior authorization on a higher percentage of claims in 2023 (more than 20 percent vs. to 17 percent in 2022). However, in certain areas, the increase was more pronounced. In Medicare Advantage (MA), for instance, 30.5 percent of claims required prior authorization in 2023 compared to 25 percent in 2022.
Despite prior authorization becoming more pervasive, the number of denials for these claims after receiving prior authorization increased across the board, often doubling or tripling the rate reported in 2022. An average of 10.4 percent of claims denied included those that were pre-approved via the prior authorization process – up from 3.2 percent in 2022.

Given that these claims were pre-approved as medically necessary prior to service delivery and almost all were eventually paid, it’s clear that the problem exists in the process of preparing and submitting a claim as well as the initial rounds of insurance review.
Providers Experience Hurdles to Clean Claim Submissions
Healthcare lacks a unified system for claims submissions, making the process of filing for reimbursement notoriously complicated. Each claim requires multiple data elements to comply, which frequently change. At the same time, each payer has its own unique rules regarding covered services, coding requirements and necessary documentation, making it difficult for providers to navigate. These inconsistencies create room for error, requiring providers to allocate more time to compliance tasks – particularly in a world where patient volumes (and the number of claims) are on the rise.
Claims submission also remains a largely manual process. This further exacerbates the problem, particularly as providers grapple with widespread staffing shortages. In fact, in a recent survey of 200 providers, every respondent indicated that staffing shortages are having a significant, negative impact on their ability to submit accurate claims for payment. Furthermore, 83 percent said staff shortages impede their ability to follow up on late payments or offer assistance to patients struggling to get services covered by insurance.
The lengthy process to adjudicate claims adds insult to injury. Even a small error can flag a claim for denial. Premier survey respondents reported that once denied, they went through an average of three rounds of reviews with insurers, with each review cycle taking between 45 and 60 days.
Payers Face Challenges Issuing Payments for Incorrect or Incomplete Claims
For payers, each claim undergoes a review for accuracy, standardization and determination of payment amounts to avoid waste, fraud and abuse, as well as payments for patients and procedures that aren’t covered by the policy.
According to leading insurers, minor clerical and/or data errors are the top reason to deny claims approved via prior authorization. Small mistakes include misspelled names, missing information, documentation and coding mistakes, and inverted numbers (i.e., social security numbers, dates of birth and other vital information). These denials are particularly frustrating, since they should be largely avoidable.
The prior authorization process is also notoriously lengthy, requiring clinical and administrative reviews of complex and varying policies. As a result, the process can take several days or even months to complete. In these cases, some providers may opt to perform what they consider to be a medically necessary service before the prior authorization has been secured, which can lead to a denial down the road.
Another problem? The need for complex and comprehensive patient records to determine the procedure’s medical necessity. Documentation often requires months of patient records including clinical notes, diagnostic test results and evidence of conservative treatments pursued before recommending more advanced care. Many providers struggle to provide this level of detail, given that patients may have seen multiple providers in multiple states for the same condition, and the lack of portability in electronic health data. Absent a complete set of records, claims may be subject to denials on the back end.
The Path Forward
Premier and our members have significant concerns about the negative effects that lengthy and cumbersome claims processes have on patients’ access to care. We continue to work with Congress and the Administration to develop appropriate policy incentives to address the root causes of delays and inappropriate denials in claims processing, removing barriers to high-quality care.
Last year, Premier and 118 of our member organizations, ranging from large health systems to independent physician offices, sent a letter to the Centers for Medicare and Medicaid Services (CMS) that included our 2024 survey results and recommended policy solutions. Premier’s survey pointed to disproportionately high rates of prior authorization use in Medicare Advantage (MA) plans compared to other insurance types, as well as disproportionately high rates of initial denials being overturned.
In part due to Premier’s advocacy, CMS provided written guidance on what MA utilization management policies are—and are not—explicitly allowed by CMS, including specific regulatory citations to better equip providers to deal with the claims appeal and contract negotiation process with MA plans. In the agency’s next MA rulemaking cycle, CMS incorporated several specific recommendations from Premier and our members, including increasing transparency in medical loss ratio (MLR) reporting to help CMS and the public monitor potentially harmful impacts from payers’ vertical integration practices.
While progress has been made, additional work remains. Premier will work with the current Administration on finalizing laser-focused policy solutions from the Contract Year 2026 MA and Part D proposed rule, such as prohibiting MA plans from reopening approved authorizations for acute care, that improve patient experiences while minimizing additional regulatory burden. Premier also looks forward to working with the Administration and Congress on developing policy solutions that unleash innovation to technology-enable current documentation, prior authorization and claims processing processes that are labor- and resource-intensive and highly susceptible to human error.
How Premier Helps Enable Faster, Easier Reimbursement
Automation and novel technologies can be used to check payer policy changes, alert staff when prior authorization is needed, gather relevant documentation and review authorization requests for accuracy. This significantly reduces staff burden and decreases the risk of claims submission without the necessary authorizations in place. These solutions also benefit payers, as increasing the rate of “clean” claims submission reduces the need for manual reviews and subsequent rounds of adjudication expense.
Premier’s solutions help bridge the gap between payers and providers – optimizing resource utilization, streamlining administrative processes, and helping to ensure accurate reimbursement and potentially improved outcomes.
- Clinical Decision Support (CDS): Our CDS technology provides real-time, evidence-based guidance at the point of care, helping providers make informed decisions, comply with medical necessity requirements and reduce the use of unnecessary services. This helps payers control costs while supporting providers in meeting value-based care goals, fostering aligned incentives and collaborative care management.
- Hierarchical Condition Category (HCC) Coding: Premier’s CodingGuide and CodingCare solutions support accurate HCC coding, promoting precise risk adjustment and appropriate reimbursement. This transparency benefits payers with reliable risk assessments while helping providers optimize revenue integrity and reduce audit risks, enhancing trust and collaboration.
- Prior Authorization (PA): Premier’s artificial intelligence (AI)-driven PA solution automates approvals using evidence-based criteria, reducing administrative burdens and delays. This enhances operational efficiency and patient access, creating a more collaborative and efficient workflow that streamlines processes for both payers and providers.
Methodology
Premier conducted a voluntary, national survey of member hospitals and health systems from August 8, 2024 to February 4, 2025. Respondents represented 280 hospitals across 23 states, accounting for over 48,000 acute care beds. Respondents were asked to consider all claims from January 1, 2023 to December 31, 2023, the last full year of completed payment data. Findings are presented as averages, weighted by acute bed capacity of the respondent. Respondents ranged in size from single-facility hospitals to large, multi-state health systems. View the survey questions here.
To calculate the costs associated with fighting payer denials, we multiplied the 3 billion claims processed each year by 0.15 (the average denial rate identified by the survey) to determine that 450 million claims were subjected to denials. We then multiplied that figure by $57.23 (the average cost incurred) to calculate $25.7 billion in costs.
Considering that 68.6 percent of these claims were ultimately paid, we multiplied $25.7 billion by 68.6 percent to calculate the costs that were largely unnecessary.

Mike is focused on driving innovation in healthcare and leading the industry through transformation by co-developing solutions with key stakeholders to help healthcare providers deliver higher quality care at a better cost.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.

Mason leads Premier’s policy development on issues related to Medicare Advantage and private insurance markets. He leverages his insurance industry expertise to support Premier’s members in the multi-payer movement to value.
Article Information

Mike is focused on driving innovation in healthcare and leading the industry through transformation by co-developing solutions with key stakeholders to help healthcare providers deliver higher quality care at a better cost.

Soumi, both a pharmacist and a lawyer, leads Premier’s Washington D.C. office. She is responsible for developing and implementing Premier’s advocacy strategy to lead the transformation to high-quality, cost-effective healthcare.

Mason leads Premier’s policy development on issues related to Medicare Advantage and private insurance markets. He leverages his insurance industry expertise to support Premier’s members in the multi-payer movement to value.